Uni-compartmental (Partial)
Knee Replacement
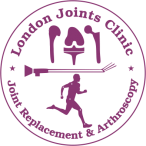
Uni-compartmental knee replacement (UKR), also called partial knee replacement, is a surgical procedure of replacing only the damaged surfaces of a single compartment of the knee due to advanced arthritis. Metal and plastic implants are used during this surgery for resurfacing of the damaged cartilage and underlying bones in one area of the knee.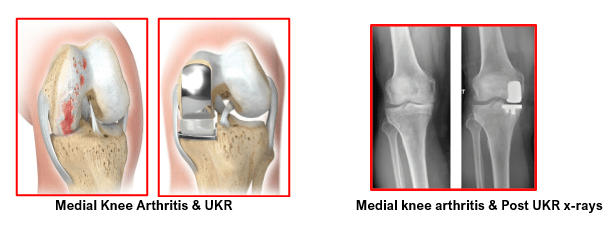
Partial knee replacement of the inner (medial) compartment is far more common than the replacement of the outer (lateral) compartment.
The replacement of the worn portions of the patella (knee cap) and the femoral trochlea(front lower portion of the thigh bone), in patients with isolated but advanced arthritis (wear) of the patello-femoral joint is also a type of partial or uni-compartmental knee replacement. This is called as patellofemoral replacement.
UKR (partial knee replacement) is typically recommended for patients:
- Having advanced arthritis of the knee limited to one side of the knee, either the medial (inner) or the lateral (outer) side
- Having intact ligaments, good mechanical stability and good range of motion in the knee
- Having healthy cartilage and bones in the non-affected compartments
- Who have previously undergone all conservative (non-surgical) treatments like lifestyle changes, painkiller medications, knee exercises, weight control, cartilage supplement medications and lubrication injection
- Whose symptoms worsen despite above measures or those who start getting serious side effects of medications
The Uni-compartmental knee replacement surgery, when done in an appropriately selected patient, offers the following advantages:
- Smaller scar
- Less tissue damage, less pain and minimal blood loss
- Faster recovery
- Short hospitalisation of 1 to 2 days only
- Knee feels more natural and has better range of motion (bends well)
- Less costly compared to a total knee replacement
The followings conditions are contra-indications for a partial knee replacement:
- Active or suspected infection in or around the knee joint
- Inflammatory arthritis like Rheumatoid arthritis
- Significant Knee stiffness
- Major deformities affecting the bones and altering its mechanical axis
- Neuro-muscular disorders affecting patient’s balance and mobility
- Obesity
- Advanced patella-femoral arthritis
- Unstable knee due to ligament insufficiency of any origin
- Untreated damage within the normal compartment
There are two types of uni-compartment (partial) knee replacements:
Mobile bearing and Fixed bearing.
Mobile bearing partial knee replacement has metallic femoral and tibial components which are fixed with bone cement. The femoral implant is curved and matches the curvature of the portion of the native femur that needs replacement. The tibial component is flat. There is a polyethylene (high grade plastic) insert that moves freely between the two metallic implants. This plastic insert is flat at the bottom and sits atop the flat surface of tibial implant. The top surface of the plastic insert matches the curvature of the femur. The femoral implant moves over the plastic insert which in turn is mobile over the smooth flat tibial component.
Proponents of mobile bearings argue that these devices provide superior conformity and improved tibiofemoral biomechanics. A more normally restored knee kinematics provides natural feeling joint along with improved range of motion. This leads to low wear rates and improved longevity (survival) of the mobile bearing implants in the long term.
In the fixed bearing implant, the plastic insert is attached and firmly locked to the tibial implant. The top surface of this plastic is curved and well contoured to match the surface of the femoral implant. The thickness (height) of the plastic insert is such that it keeps the knee ligaments stable and allows good range of movement. The advocates of fixed bearing implants argue for technical ease in implantation, especially as regards to ligamentous balancing.
Steps involved in a partial knee replacement surgery:
Anaesthetic
- The mini knee may be performed under epidural, spinal or general anaesthesia. We usually prefer epidural anaesthesia since a good epidural can provide up to 48 hours of post-operative pain relief and allow faster, more comfortable progress in physiotherapy.
- Minimally invasive partial knee replacement surgery begins by performing a sterile preparation of the skin over the knee to prevent infection followed by inflation of a tourniquet to prevent blood loss during the operation.
- A small skin incision, about 3-4 inches in length, is made alongside the patella (kneecap) and the knee joint is exposed. The joint is then thoroughly inspected to confirm that the arthritis is principally confined to one side of the knee and the other compartments are healthy.
- If there is significant cartilage damage to the under-surface of the patella (kneecap) or on the opposite side of the knee, a partial knee replacement is unlikely to provide durable pain relief. In such cases, a longer incision is then made, and a traditional total knee replacement is performed. This change in plans may be needed for about 10 percent of patients who are initially posted for partial knee replacement.
- This decision to convert from a partial knee to a total knee replacement needs good judgment and a highly experienced surgeon. Proper patient selection is essential for good outcomes in all types of knee surgery, but this is especially true for the partial knee replacements. Patients must be pre-counselled about intra-operative change of plans and consent taken accordingly.
- After confirmation of arthritis localised to a single compartment only, specialized alignment rods and cutting jigs are used to remove enough bone from the end of the femur (thigh bone) and the top of the tibia (shin bone) to allow placement of the partial knee replacement implants. Proper sizing and alignment of the implants are critical for normal post-operative function and good pain relief. These steps are critical and considerable experience in minimally invasive partial knee replacement is required in order to make sure they are done reliably case after case.
- Trial implants, of appropriate sizes, are placed without bone cement and checked for their fit against the cut bony surfaces. The knee is now checked for overall limb alignment, ligament balance and stability, range of knee motion i.e flexion (bending) and extension (straightening) and patellar tracking. After checking all the above factors, the trial implants are now removed. OT assistants are asked to keep the real implants, the same size as the trials, ready for implantation.
- The cut bony surfaces of the femur and tibia are then cleaned with saline solution using a special pulse lavage device and then dried thoroughly.
- The selected femoral and tibial implants are cemented into place using bone cement. The plastic insert between the metallic femoral and tibial implant could be a mobile bearing type or a fixed bearing type. (The type of implant selected depends on the pre-operative planning, patient counselling and the experience and preference of the operating surgeon).
- Once all definitive implants are in place, the wound is given a final wash and the surgical incision is closed using sutures and staples. A sterile dressing is placed over the wound and a compression bandage is applied.
- The average time needed for completion of partial knee replacement surgery is between 50 to 60 minutes.
- Patients are allowed to eat and drink, 2 to 3 hours after completion of surgery. They are monitored in the recovery room and shifted to their ward bed once they are stable. This stay in the recovery ward can be for 1 to 2 hours.
- Epidural anaesthesia is continued post-surgery for 24 to 48 hours. If there is any breakthrough pain, then intra-venous paracetamol and or diclofenac injections are given for first 24 hours. This can be changed to oral analgesics on the next day. Oral painkillers are taken regularly for the first 5 to 7 days and then as required.
- 2 additional intra-venous antibiotic doses are given at 8 hourly intervals. Patient’s blood samples are taken next morning to check their haemoglobin, urea, creatine and electrolyte levels. Iron supplements are started if the Hb is low (<10).
- Patients are provided ice packs regularly which helps reduce knee swelling and keeps pain under control. They are encouraged to start moving their toes and ankle as soon as their anaesthesia wears off. If tolerated they can do straight leg raising intermittently. They can start full weight bearing, with help of a walker or a pair of elbow crutches, either the same day evening or the next morning. Patients are trained to get in and out of their bed by themselves, use the commode, use the stairs and also sit in a chair. Range of motion knee exercises are done as tolerated. They are given blood thinning medications daily during their indoor stay. Then oral medications are given for 2 weeks.
- Once patients become safely mobile and are relatively pain-free, they can be discharged home on the 2nd or 3rd Their dressings are changed prior to the discharge. These new dressings are left undisturbed for 2 weeks until suture removal. Patient’s wound gets checked and the sutures/staples are removed 14 days after surgery. Patient can start taking normal bath after this. Bathing prior to suture removal are allowed with waterproof covering of the surgical site and precautions are taken to avoid the wound getting wet.
- Normal breakfast and routine diet are allowed from the next day of surgery. Patients are encouraged postoperatively to eat healthy food including green leafy vegetables and fruits. Vitamins and iron supplements make be prescribed if needed.
- Physiotherapy is essential for the first 4 to 6 weeks post-surgery and may need to be continued for 2 to 3 months. This can be done in the hospital on OPD basis or by having home physiotherapy sessions under supervision of an experienced physiotherapist. Physiotherapy helps in quick recovery of knee range of motion, muscle strength and knee function. Ice packs are also used regularly for 4 to 6 weeks after discharge. Most patients are pain-free and able to walk unaided around 4 to 6 weeks after partial knee replacement. Patient’s recovery is, typically, much faster and they have less pain compared to a total knee replacement.
- Office type work can be started after 2 to 3 weeks. Car driving can be started by the 4th postop week.
- Patients are encouraged to remain active and do their exercises. They can do walking, swimming, cycling, light tennis etc. But high impact activities like jogging/ running are NOT advisable and should be avoided.
Uni-compartmental knee replacement is a highly successful operation in appropriately selected patient population. The operation has been perfected over time with the introduction of new prosthetic designs and the development of instrumentation that allow precise implantation through limited incisions.
The overall survival rate at 10 to 12 years post-surgery is about 95 to 98 %. These survival rates are almost similar for the mobile bearing and the fixed bearing types of UKRs. Patients are freely mobile without pain. They are able to lead an active and independent lifestyle. Their knee too feels near normal and has good range of motion.
The possible risks and complications after uni-compartmental (partial) knee replacement are as follows:
Risks for any anaesthesia are:
Allergic reactions to medicines
Breathing problems
Risks for any surgery are:
Blood clots in the legs (DVT- deep vein thrombosis) that may travel to the lungs (PE- pulmonary embolism)
Infection, including in the lungs, urinary tract, and chest
Bleeding
Possible complications after UKR:
Infection of the knee joint
Wear of the artificial joint
Loosening of the artificial joint over time
Dislocation of the mobile bearing
Fractures around the implants
Inflammatory synovial disease progression (lipoma arborescens)
Knee stiffness
Allergic reaction to the artificial joint – rare
Injury to nerves, blood vessels or surrounding knee ligaments.
Need for revision surgery in the future for any reasons including progression of arthritis in the unaffected knee compartments.
People who have a prosthesis, such as an artificial joint, need to carefully protect themselves against infection. You should carry a medical identification card in your wallet that says you have a prosthesis. You may need to take antibiotics before any dental work or invasive medical procedures.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :