Shoulder Slap Tears
& Management
The shoulder is the most mobile joint in the body. This requires a complex arrangement of structures to keep the shoulder joint stable during its various movements.
Excessive shoulder mobility puts the shoulder structures at risk of injury which can affect the stability of the shoulder.
The glenoid (shoulder socket) is a very flat cup and as such, it is inherently unstable. The glenoid has a rim of fibrous cartilage all the way around its periphery. This is called the labrum. It deepens the socket and provides some stability. This stability is additionally reinforced by capsular thickenings called as ligaments.
The long head of biceps tendon is a cord like structure that arises from the top of the glenoid. It’s attachment blends firmly with that of the labrum.
SLAP tear is an acronym for Superior Labrum Anterior to Posterior tear. The top portion of the labrum gets detached from the upper most part of the glenoid rim. This may or may not involve the biceps attachment.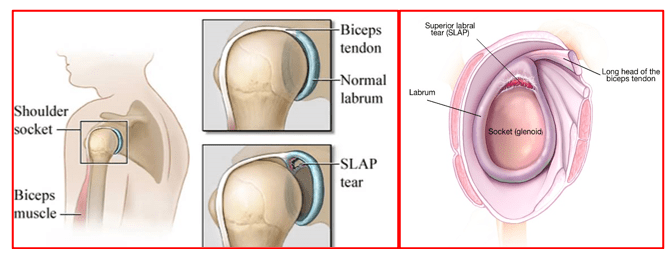
SLAP tears can occur as a result of trauma or chronic overhead activities.
A fall on an outstretched hand with a tensed biceps or a fall directly onto the shoulder are thought to be the most common mechanism of injury.
SLAP tears can also occur after shoulder dislocations along with other labral injuries.
Chronic / Repetitive overhead activities, during sports or work, cause forceful rotatory movement of the shoulder. This type of movement can pull on the Long Head of Biceps (LHB) Tendon. This creates traction force on an area called biceps anchor which consists of the attachment of the long head of biceps to the top of the glenoid and the surrounding upper labrum. Repeated overhead activities ultimately cause the superior labrum to detach, from the upper part of the glenoid, leading to a SLAP tear.
Overhead athletes e.g. baseball-pitchers and tennis players, are particularly prone to SLAP injuries.
SLAP tears can be associated with shoulder instability, articular sided rotator cuff tears, internal impingement, GIRD (gleno-humeral internal rotation deficit) and scapular dyskinesia.
Disturbed biomechanics of the shoulder joint, due to muscular imbalances, creates tension on the superior labrum and causes it to peel off or tear from the top surface of the glenoid.
SLAP tears are diagnosed based on patient’s history, symptoms and clinical examination. It is confirmed on an MRI scan of the affected shoulder. MRI helps in the assessment of SLAP tear, presence of any additional labral injuries, status of the rotator cuff, long head of the biceps and the surrounding bones and joints.
Patients may give history of feeling of a popping sensation during injury or overhead activity. They have pain deep within the shoulder joint. They also have difficulty with overhead or throwing activities.
Patients have pain especially when their arm is held across the chest and rotated. There may be clicking or popping sound noted during shoulder examination in overhead position. Such patients may also have reduced internal rotation of the affected shoulder and wasting of shoulder muscles due to suprascapular neuropathy.
If these patients have additional lower labral injury, then they may show signs of apprehension on stressing of the shoulder. They may feel that their shoulder is about to dislocate.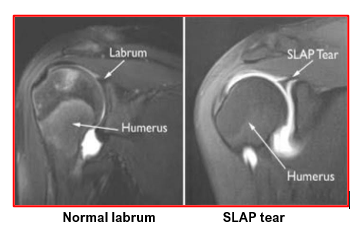
SLAP tears have been classified based on the nature of the tear:
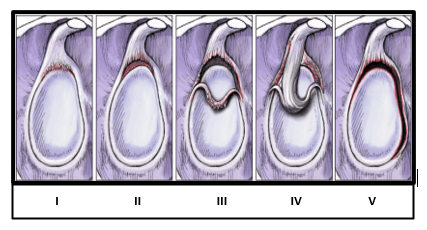
- Type I Frayed but without any true detachment. This is often a
degenerative condition affecting many middle aged or elderly
patients
- Type II Traumatic detachment of the biceps anchor
- Type III Longitudinal mid-substance tear of the superior labrum that forms a
bucket-handle tear
- Type IV Mid-substance tear of the superior labrum, which extends into the
substance of the biceps tendon.
- Type V Mid-substance tear which extends anteriorly into a Bankart lesion
(Maffet classification)
There are a number of treatments available for recurrent instability, however the treatment has to be specific for the nature of the instability.
The options include:
- Use of painkiller and anti-inflammatory medications as required
- Activity modifications until pain settles down
- Physiotherapy exercises help to improve core strength, the shoulder blade position as well as the strength of the rotator cuff. This leads to optimisation of the muscles that aid shoulder stability and also help in reducing shoulder pain.
- Patients who have failed to respond to non-surgical treatment of 3 to 4 months duration are offered surgery.
Arthroscopic surgery for SLAP repair:
- Typically, an arthroscopic SLAP repair surgery involves insertion of 1 to 2 suture anchors at the top of the glenoid, freshening of labrum attachment site to promote healing, passing of the sutures around the detached labrum and tying of the suture knots to complete the SLAP repair. If there are tears extending into lower labrum, both at the front (anterior) or at the back (posterior), then these are also repaired in a similar manner (Bankart Repair).
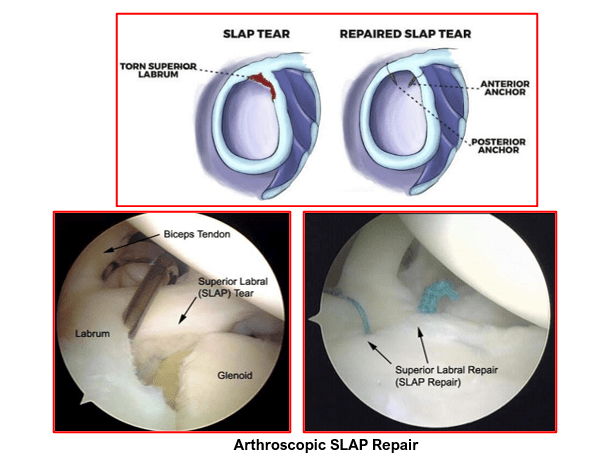
- If the biceps tendon too is detached from the glenoid and has good tissue quality, it is cut at the top and the cut tendon is re-attached at a new location on the upper humerus with an additional suture anchor. This is called Biceps Tenodesis. This stops the traction force exerted by the long head of the biceps on the superior labrum.
- Only arthroscopic debridement is needed in cases where the SLAP is frayed, and the biceps anchor is not detached.
- In cases where the SLAP is torn, displaced and of poor quality, it is just debrided followed by biceps tenodesis (younger patients < 50 years) or tenotomy (>50 years old patients)
- Patients are advised to take pain-killer medications as and when needed. They are forewarned that SLAP repairs tend to be more painful.
- Shoulder sling is given for 4 to 6 weeks
- They need to do ice-packing of the shoulder region 4 to 5 times a day
- Portal wound sites are kept dry. Armpit area is kept dry and clean when using the shoulder sling to avoid blister formation due to sweating. Talcum powder is recommended.
- Pendulum exercises are started on the same day of the surgery and are continued for 4 weeks. After 4 weeks, active and active assisted range of motion exercises are started to get back normal shoulder mobility.
- Overhead activities and excessive external rotation are avoided for 6 weeks.
- Shoulder strengthening exercises are started gradually after 6 weeks.
- Majority of patient have good shoulder strength and mobility by the end of 3 to 4 months. They can now start sports specific training. Full active unrestricted activities are allowed after 4 to 6 months.
The SLAP repair surgery involves certain potential risks and complications:
- Wound infection
- Swelling around the shoulder
- Excessive bleeding and bruising around the shoulder
- Blood clots formation
- Shoulder stiffness
- Injury to the nerves or blood vessels
- Damage to the articular surfaces of the humeral head (ball) or the glenoid (socket)
- Hardware failure and pull-out of the suture anchors
Some patient’s activities may not return to full pre-injury levels
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

