Home >> Shoulder Services
Shoulder Instability
and Dislocations
The shoulder joint is a ‘ball and socket joint’ with a shallow socket (glenoid) and a large hemispherical ball (head of humerus) which makes it unstable.
A fibro cartilage tissue called the labrum (lip in Latin) is attached to the circumference of the glenoid. The labrum helps to deepen the shallow socket and form a type of suction cup for the ball.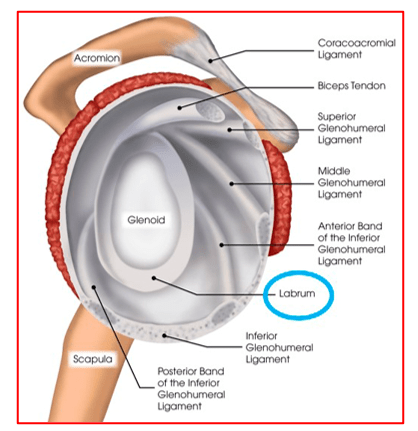
The lining of the joint (shoulder capsule) is very loose which allows excellent mobility to the ball. 3 types of capsular ligaments (superior, middle and inferior glenohumeral ligaments), that are thick cord like structures from the capsule to the labrum, provide additional stability. These ligaments help in keeping the shoulder joint stable throughout its range of motion.
Shoulder Instability is a term describing abnormal looseness of the shoulder joint, such that the ball part of the joint (humeral head) slides out of the socket (glenoid).
It is a pathological condition, rather than a normal physiologic variant such as laxity – looseness.
A minor form of instability in the shoulder joint is called Subluxation wherein the shoulder ball partially slips out of the socket.
A more severe case of instability can cause the shoulder to completely slip out its socket and is known as a Dislocation.
Shoulder instability can develop in two different ways.
Traumatic (injury related) or Atraumatic Instability
Traumatic instability – If the ligaments holding the shoulder ball in its socket become stretched or torn due to trauma or overloading, the necessary stability of the ligaments throughout the shoulder’s large range of motion is compromised.
In Atraumatic instability there is a general laxity (looseness) in the joint that eventually causes the shoulder to become unstable.
Understanding the differences in shoulder instability is essential in choosing the best course of treatment.
A fall on an outstretched arm that is forced overhead, a direct blow on the shoulder, or a forced external rotation of the arm are frequent causes of anterior (forward) dislocation. This is the commonest type of dislocation.
An epileptic seizure attack or electrocution generates severe abnormal muscular forces around the shoulder which causes posterior (backward) dislocation.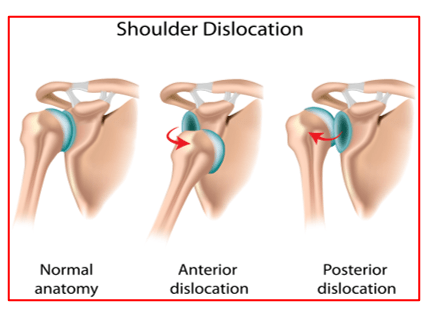
Patients give a history of trauma followed by immediate onset severe shoulder pain and a sense of shoulder popping out of socket. They have difficulty in moving the arm. Patients may complain of swelling, deformity, numbness or weakness.
Shoulder dislocation is diagnosed based on patient’s history of injury, thorough clinical examination and x-rays.
A patient with shoulder dislocation usually holds the arm still against his side and any attempts to move the shoulder are painful. A large crease under the acromion (tip of shoulder) and a bulge in the armpit are clues to the direction of the dislocation. Range of motion, strength, and sensation will be tested if possible. Any changes or loss of sensation may point towards a nerve damage. The physician will also check the pulses in your arm in order to detect the possibility of vascular complications.
In those cases where the shoulder has managed to relocate spontaneously, the diagnosis can be difficult. Patients may only report the feeling of the shoulder “slipping out” before the spontaneous reduction occurred.
X-rays of the shoulder joint are usually taken to confirm the dislocation, its direction, and to check for a related fracture.
X-rays may reveal a ‘bony Bankart’, which is a fracture of the anterior-inferior glenoid (front, lower portion of the glenoid).The presence of this fracture indicates that the labrum and ligaments in the front part of the shoulder are no longer attached to the glenoid.
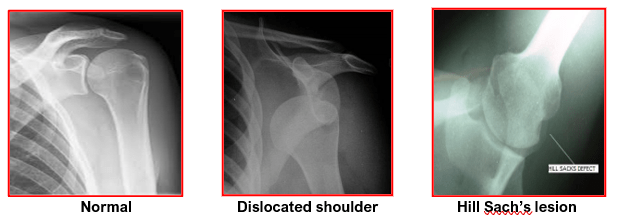
X-rays will also show an impaction fracture of the head of humerus in the posterolateral aspect. This lesion is called as the Hill Sach’s lesion.
After confirming shoulder dislocation by clinical examination and x-rays, the patient is given sedation or a general anaesthesia to relax the muscles around shoulder region. With the help of an assistant the doctor will give gentle traction and manipulate the arm to relocate the shoulder joint. This is called as closed reduction. X-rays are done again after reduction to confirm that the joint is relocated in place.
Patient’s pain is immediately relieved after shoulder reduction. A shoulder sling is given for support and comfort. The sling is to be used for 2-4 weeks.
On discharge, the patient is advised to see a Shoulder Specialist for follow-up and additional investigations like a shoulder MRI and CT scans. Meanwhile only gentle pendulum exercises are allowed until first follow-up.
Recurrent dislocations are most common in young people, athletic people and those involved in heavy physical activities.
The younger and more active the patient is at the time of first dislocation, the more likely it is that recurrent instability will develop. For example, if the first dislocation occurs during the teenage years, there is a 70-90% chance that recurrent instability will develop. However, people over 40 years of age with a first dislocation have less than a 10% risk of developing recurrent instability.
Chronic shoulder instability is caused by:
- Traumatic shoulder dislocation:
The labrum, which deepens the socket, is torn and the capsular ligaments, which hold the shoulder ball in its socket, become stretched or torn. As a result, the necessary stability of the ligaments throughout the shoulder’s large range of motion is compromised.
- Repetitive overhead activities:(as seen in sports like Swimming, tennis, and volleyball) can stretch out the shoulder ligaments due to chronic overloading. Similar things happen to people in jobs needing repetitive overhead work. These loose ligaments cannot support the humeral head within the socket. Such patients will develop shoulder instability and pain when doing repetitive stressful activities.
- Multidirectional Instability:
In a small group of patients, the shoulder can become unstable without any history of injury or repetitive strain. These patients have naturally loose ligaments throughout the body and may be “double-jointed.” The shoulder can dislocate in many directions. Hence it is called Multi-directional instability (MDI). Such patients can produce a shoulder dislocation (voluntarily) at will without pain.
Common symptoms of chronic shoulder instability include:
- Pain caused by shoulder injury
- Repeated shoulder dislocations
- Repeated instances of the shoulder giving out
- A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just “hanging there”
After taking a detailed medical history, the surgeon performs a thorough clinical examination of the shoulder to diagnose instability.
Investigations like x-rays and MRI of shoulder are then done to confirm the underlying pathologies.
X-rays will show fracture of rim of glenoid – Bony Bankart’s Lesion & impaction fracture of humeral head – Hill Sach’s lesion
MRI will show: Rotator cuff tears, lesions of biceps tendon, Avulsion of labrum and capsular ligaments from the glenoid – Soft tissue Bankart’s lesion, capsular avulsion from humerus
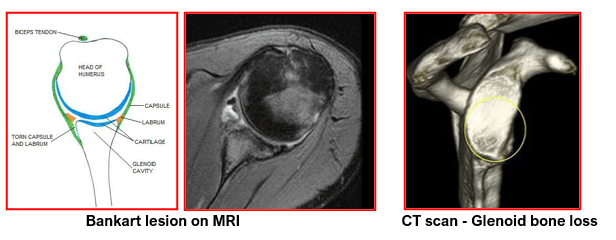
CT scan may be required in cases where damage to the glenoid is noted on x-rays. This helps understand the nature and extent of bone loss on the glenoid and the humeral head.
Treatment for shoulder instability is based on a variety of factors including the severity of the condition, and the patient’s age, activity level, occupation, and natural degree of looseness in the joint.
Dr. Jadhav will plan your definitive treatment (conservative or surgical) after taking all above factors into consideration.
Initial treatment for any shoulder instability relies on physiotherapy, activity modifications and painkillers as required.
Strengthening the rotator cuff muscles and the periscapular muscles (those around the scapula) gives stability to the joint. The goal of physiotherapy is to help the muscles provide stability to the shoulder that the torn ligaments are not able to provide. The physiotherapy is carefully designed for each patient since this condition often causes apprehension about certain arm positions or exercises. Often physiotherapy can help regain lost motion, reduce apprehension, and restore shoulder function.
Changes to lifestyle and modification of activities are necessary to avoid repetitive stress to the shoulder and to resolve symptoms.
Surgery is usually recommended if recurrent instability cannot be controlled even after adequate physiotherapy and activity modification.
Surgery is recommended after the first dislocation in young persons (< 20 years) who have a higher risk of re-dislocation, in contact athletes who plan on continuing to participate in sports that put their shoulders at risk and in people involved in heavy physical activities.
The shoulder becomes stable which improves patients’ confidence, shoulder strength and function. The stabilization surgery allows them to return to normal work or sporting activities. It also prevents further damage to the surfaces of ball and socket due to repeated instability.
Shoulder instability surgery is a surgical attempt to reconstruct the normal shoulder anatomy by repairing the torn cartilage ring (labrum) and re-tensioning the stretched capsular ligaments without over tightening. The aim of surgery is to return stability to the shoulder with the least loss of motion. This can be achieved either by arthroscopic or open techniques. This procedure is known as the Bankart Repair.
Depending on the extent of damage to the labrum, 2 to 3 suture anchors (metallic or non-metallic) may be buried at different locations on the rim of glenoid (socket). Non-absorbable sutures that are pre-loaded on these anchors are then shuttled through the avulsed capsular labral tissue. Then these sutures are tied, from bottom to top, to repair the labrum to its normal place. This recreates the normal labrum bumper effect, and also re-tensions the capsular ligaments. At the end of the procedure, the humeral head is seen getting centralised over the glenoid and it remains stable when checking the stability and mobility of the shoulder joint.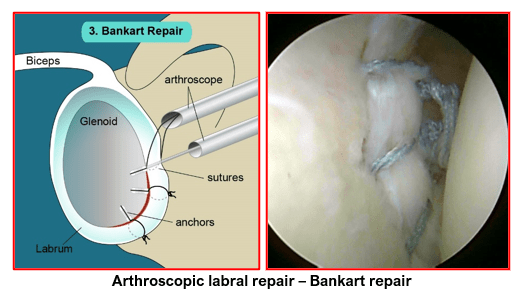
Arthroscopic shoulder stabilization (Bankart Repair) is done using a fibre-optic telescope, camera and specialized instruments via 3 to 4 tiny scars.
Dr Jadhav has specialised in these arthroscopic shoulder stabilisation surgeries for managing different types of shoulder instabilities and dislocations.
Arthroscopic shoulder stabilisation has the following advantages:
- Small scars give better cosmetic result
- Minimal tissue trauma and pain
- Less bleeding
- Shorter hospitalization
- Excellent visualization of shoulder joint and the associated lesions of instability
- Additional shoulder pathologies like rotator cuff tears or biceps tendon lesions can be dealt with at the same operation
- Can give same success rate as that with open stabilization surgery
- Faster recovery
The Latarjet procedure (also known as the Latarjet-Bristow procedure) is a surgical procedure used to treat recurrent shoulder dislocations, typically caused by bone loss or a fracture of the glenoid. The procedure was first described by French surgeon Dr Michel Latarjet in 1954.
The Latarjet procedure is performed either by open technique or arthroscopic technique for patients who have more than 15 to 20% glenoid bone loss as confirmed on CT scans.
It involves the removal and transfer of a section of the coracoid process and its attached tendons to the front of the glenoid. This bone block is fixed flushed to the front of the lower glenoid region with 2 special screws. It fills up the area with usual glenoid bone loss due to recurrent dislocations and increases the glenoid width.
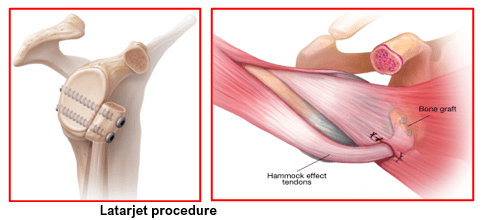
The mechanism of action of the Latarjet procedure has been described as a Triple Blocking Effect which stabilises the shoulder and prevents further dislocations:
- Increasing or restoring the width or arc of the glenoid bone
2) Sling effect of the Conjoint tendon on the subscapularis and capsule
whenever the arm is in the abducted and externally rotated position. The
conjoint tendon supports the humeral head and avoids dislocations.
(This is the arm position in which shoulders dislocate frequently. E.g. when
doing overhead activities or throwing activities and also during sleeping).
3) Repair of the capsule to the stump of coracoacromial ligament. This step re-tensions the capsules and provides stability against dislocations.
The Latarjet procedure is best suited as the shoulder reconstruction procedure of choice for:
- contact athletes, rugby players, wrestlers and heavy manual workers
- patients with increased shoulder laxity (generalised hyperlaxity)
- patients with failed previous shoulder reconstructions & poor tissues
- patients with significant bone damage to the glenoid & humeral head
It has the advantage of maintaining external rotation movement of the shoulder and also allows participation in sporting activities.
With appropriate patient selection, the Latarjet procedure can be expected to prevent recurrent anterior instability in approximately 94-99% of cases.
Remplissage is a French term which means ‘to fill-in’.
Remplissage procedure is an arthroscopic shoulder surgery that is performed for treating recurrent anterior shoulder dislocations in patients, who have a large engaging Hill Sach’s defect of the humeral head along with a Bankart lesion of the glenoid. Such patients have unstable shoulders. Whenever the arm is in abducted and externally rotated position, the Hill Sach’s lesions catches against the anterior rim of the glenoid and dislocates easily.
In arthroscopic remplissage procedure, the infraspinatus tendon and posterior capsule are tied down with suture anchors to fill in the engaging defect of the humeral head. This makes the intra-articular Hill Sach’s lesion into an extra-articular one and stops it from engaging with the front rim of the glenoid with overhead activities.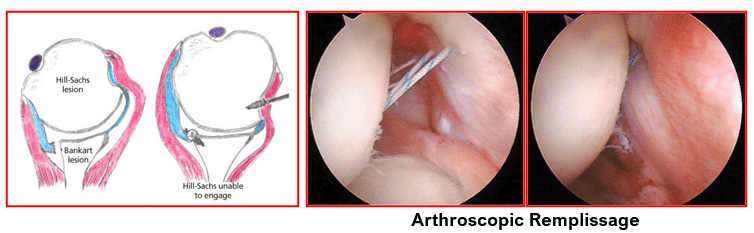
Remplissage procedure is routinely combined with anterior Bankart repair to stabilise unstable shoulders and reduce the incidence of recurrent anterior shoulder instability.
But it does have the risk of limiting patient’s external rotation at the shoulder. Hence, remplissage procedure is not recommended for patients who need full external rotation of their shoulders for sports related or occupational activities. e.g. throwers & fast bowlers.
Open shoulder stabilisation is useful in the following situations:
- There is co-existing fracture of the socket (glenoid) or humeral head
- Glenoid is worn out into an inverted pear shape due to recurrent anterior instability
- Failure of previous shoulder stabilization surgery
- Surgeon is not experienced in arthroscopic stabilisation techniques
- Capsular tissue is not repairable and needs transfer of a bony block with attached soft tissues (Latarjet procedure) or an iliac crest bone block transfer.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

