Home >> Shoulder Services
Shoulder Arthritis &
Shoulder Joint Replacements
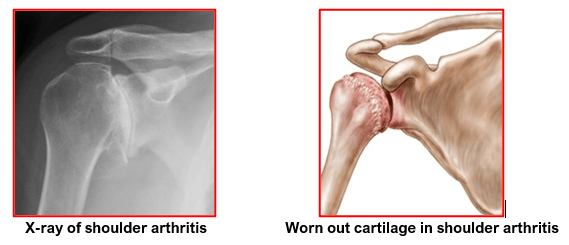
Shoulder joint arthritis is a condition wherein the smooth joint cartilage is damaged and worn out.
Common causes for shoulder arthritis:
- Osteoarthritis
Osteoarthritis, or ‘wear-and-tear’ arthritis, is a degenerative condition that destroys the smooth outer covering (articular cartilage) of bone. It usually affects people over 50 years of age and is more common in the acromioclavicular joint than in the glenohumeral shoulder joint.
- Rheumatoid Arthritis
Rheumatoid arthritis is an auto-immune systemic inflammatory condition of the joint lining, or synovium. It can affect people of any age and usually affects multiple joints on both sides of the body.
- Post-traumatic Arthritis
Post-traumatic arthritis is a form of osteoarthritis that develops after an injury, such as a fracture or dislocation of the shoulder. Arthritis can also develop after a rotator cuff tear.
- Avascular necrosis (AVN)is a condition in which the bone of the humeral head dies due to lack of blood supply. Chronic steroid use, deep sea diving, severe fracture of the shoulder, sickle cell disease and heavy alcohol use are risk factors for avascular necrosis
The most common symptoms of shoulder arthritis are joint pain, stiffness and weakness.
The shoulder is pain is aggravated by activity and progressively worsens. If the glenohumeral shoulder joint is affected, the pain is localised to the back of the shoulder and may intensify with changes in the weather.
Stiffness or Limited motion is another symptom. It may become more difficult to lift your arm to comb your hair or reach up to a shelf. You may hear a clicking or snapping sound (crepitus) as you move your shoulder. There may be associated weakness of shoulder muscles.
As the disease progresses, any movement of the shoulder causes pain. Night pain is very common, and sleeping may be difficult.
The diagnosis of shoulder arthritis is made on the basis of patient symptoms, detailed medical history, thorough clinical examination and appropriate investigations.
- Weakness (atrophy) in the muscles
- Tenderness to touch
- Extent of passive (assisted) and active (self-directed) range of motion
- Any signs of injury to the muscles, tendons, and ligaments surrounding the joint
- Signs of previous injuries
- Involvement of other joints (an indication of rheumatoid arthritis)
- Crepitus (a grating sensation inside the joint) with movement
- Pain when pressure is placed on the joint
X-rays of an arthritic shoulder will show a narrowing of the joint space, changes in the bone, and the formation of bone spurs (osteophytes).
CT and MRI scans may be used to ascertain the severity of bony deformities, the amount of bone loss and the status of the soft tissues, especially the rotator cuff tissue.
If an injection of a local anaesthetic into the joint temporarily relieves the pain, the diagnosis is supported.
Initial treatment for arthritis of the shoulder is non-surgical and may involve physiotherapy.
- Rest or change activities to avoid provoking pain. You may need to modify the way you move your arm to do things.
- Physiotherapy:may be helpful when arthritis is in early stages. It helps maintain joint motion and strengthen the shoulder muscles.
- Moist heat
- Anti-inflammatory and pain-killer medications:to reduce pain and inflammation
- Icethe shoulder for 20 minutes two or three times a day to reduce inflammation and ease pain
If you have rheumatoid arthritis, your doctor may prescribe a disease-modifying drug, such as methotrexate, or recommend a series of corticosteroid injections.
Shoulder arthroscopy surgery is useful only during the early stages.
With this operation, the doctor will trim out the inflamed synovial lining tissue and remove debris and pieces of degenerated cartilage. This surgery can relieve many of the symptoms, at least for a while. Patients must always be counselled that arthroscopic surgery does not cure arthritis and the benefits from surgery are not permanent.
Shoulder replacement surgery is recommended if:
- There is moderate or severe shoulder pain that limits one’s everyday normal activities of daily living.
- No improvement in pain after taking regular pain killers.
- Harmful side-effects from pain-killer medications
- No improvement in pain even after Modification / restriction of activities
- When there is no improvement with physiotherapy.
- X –rays confirming advanced shoulder (glenohumeral) arthritis.
- Shoulder replacement is also recommended for previous surgeries like failed fracture fixation or failed shoulder replacement as a revision (re-do) surgery.
Shoulder replacement is not advised if there is:
- Active or recent infection
- Paralysis of deltoid or rotator cuff muscles
- Neuropathic Joint (Charcot Joints)
- Glenoid resurfacing is not done if massive rotator cuff non-repairable tears
In a shoulder replacement surgery, the painful surfaces of the damaged shoulder are replaced with artificial shoulder parts. The part that replaces the ball consists of a stem with a rounded highly polished metal head. The part that replaces the socket consists of a durable smooth plastic concave shell that matches the round head of the ball.
There are several different types of shoulder replacements:
- Shoulder Hemiarthroplasty:This is partial shoulder replacement wherein only the humeral head (ball part) of the shoulder joint is replaced. The glenoid (socket) is not replaced if it has good cartilage.
Sometimes, the decision to perform total shoulder arthroplasty or hemi-arthroplasty is made in the operating room at the time of the surgery.
Implantation of a glenoid component is not advised if:
- The glenoid has good cartilage.
- The glenoid bone is severely deficient.
- The rotator cuff tendons are irreparably torn.
- Total Shoulder Replacement:involves replacing the arthritic joint surfaces with a ball attached to a stem, and a plastic socket. Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are generally good candidates for conventional total shoulder replacement.
The shoulder replacement components come in various types and sizes. If the bone is of good quality, your surgeon may choose to use a non-cemented or press-fit humeral component. These implants have a special porous coating which allows bone to grow into it to give lasting stability.
If the bone is soft, the humeral component may be implanted with a special glue (bone cement). In most cases, the all-plastic glenoid component is implanted with bone cement.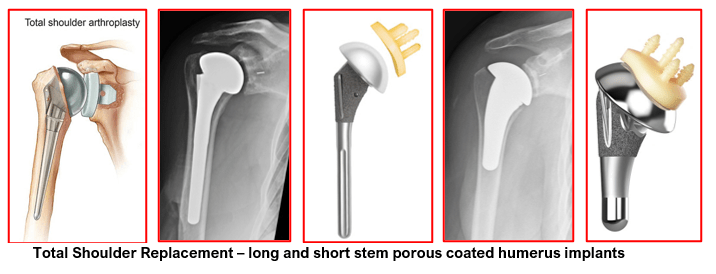
Reverse total shoulder replacement:
Another type of shoulder replacement is called reverse total shoulder replacement. This surgery was developed in Europe in the 1980s.
Reverse total shoulder replacement is used for people who have:
- Completely torn rotator cuffs and the effects of severe arthritis (cuff tear arthropathy)
- Had a previous shoulder replacement that has failed
- Had a previous upper humerus fracture fixation that has failed
- Had severe multi-fragmented fractures of the upper humerus that are difficult to reconstruct
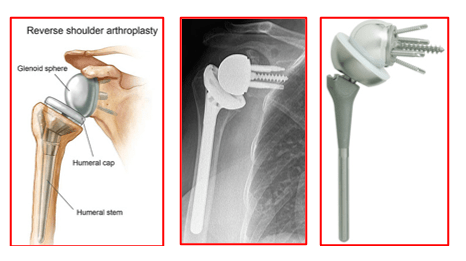
In Reverse shoulder replacement surgery, the positions of ball and socket are reversed.
The ball is fixed to the shoulder blade at the glenoid and is stationary. The socket is mounted on a stem inserted into the upper end of humerus bone and is mobile.
The reverse shoulder replacement needs an intact deltoid muscle for shoulder movements!
Shoulder Resurfacing Surgery is an alternative to conventional shoulder replacement for the treatment of shoulder arthritis. It provides a bone conserving shoulder hemi-arthroplasty.
Shoulder resurfacing surgery involves relining rather than replacing the damaged ball of shoulder joint.
During this surgery, only the damaged cartilage from the head of the humerus is removed, along with very minimal amount of normal bone from the neck of humerus.
The humeral head is then relined with a metallic cap that is either fixed with bone cement or an uncemented metallic cap which has a special coating on its inner side. Uncemented implant encourages bony ingrowth to provide fixation and stability.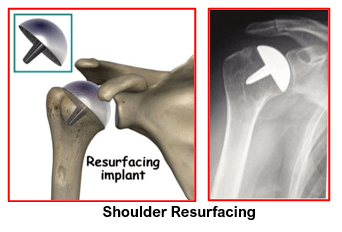
Total Shoulder Replacement is considered as successful (95%) in relieving pain as total hip or knee replacement.
Patients have an improved quality of life after shoulder joint replacement surgery. Their pain is abolished or significantly reduced. They have improved motion, better strength and better function.
Risks associated with Shoulder Replacement are:
- Stiffness
- Infection
- Axillary nerve injury – recovers as mostly neuropraxia
- Peri-prosthetic fractures
- Rotator cuff tears
- Glenoid loosening
- Instability
Patient’s progress after his shoulder replacement surgery should be as follows:
- Hospital stay is for 1 to 2 days.
- After surgery, the arm is kept in a shoulder sling for support and comfort.
- Shoulder sling is required for 6 weeks until soft tissue healing occurs.
- A pillow is used under the elbow for support when sitting and also when sleeping
- From the day of operation movements of fingers, wrist and elbow are encouraged.
- For the first six weeks patients are only allowed pendulum exercises and passive assisted exercises out of sling. This allows good tissue healing without causing stiffness. They should do the exercises thrice a day.
- Wound healing is checked 10 days after surgery and any sutures removed
- 6th to 12th weeks: Gradual improvement in range of motion is started. Active exercises are encouraged.
- After 12th weeks: Strength straining starts to build on gains from previous weeks. The physiotherapist will use different modalities to improve the strength of your shoulder muscles.
- Physiotherapy must be continued for 6 to 12 months post-operatively for maximum benefit of shoulder replacement surgery.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

