Rotator Cuff Lesions
& Management
The rotator cuff is a specialised structure of four muscle-tendon units that fuse together and surround the front, back, and top of the shoulder joint just like the cuff of a shirt sleeve. These tendons play an important role in joint function by helping in stabilising the shoulder joint throughout activities of daily living, as well as allowing shoulder rotations and overhead arm movements.
The tendons making up the rotator cuff arise from these muscles: supraspinatus, infraspinatus, teres minor and subscapularis.
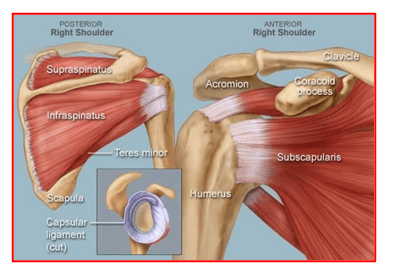
Supraspinatus – this muscle sits on top of the shoulder blade. Its tendon runs over the top of the humeral head. This is the tendon that is most commonly inflamed or torn.
Infraspinatus – this muscle is at the back of the shoulder below the spine of the shoulder blade. Its tendon is attached to the back of the humeral head and helps in turning the arm outwards
Teres Minor – Arises from the lower part of shoulder blade below the infraspinatus. It is the smallest muscle of the rotator cuff and helps in outward rotation of the arm along with the infraspinatus.
Subscapularis – This muscle arises from the front of the shoulder blade and its tendon crosses the front of the shoulder joint. It helps in inwards rotation of the arm.
The following problems that can arise in any of the rotator cuff tendons:
Tendinitis, Partial tears & Full thickness tears
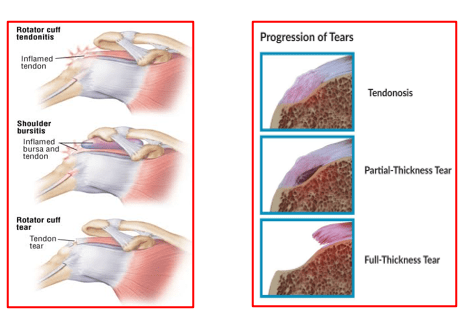
- Tendinitis: This is tendon inflammation that can occur be due to trauma and stretching of tendon without tears, due to friction and pinching of the tendon or deposition of calcium within the tendon
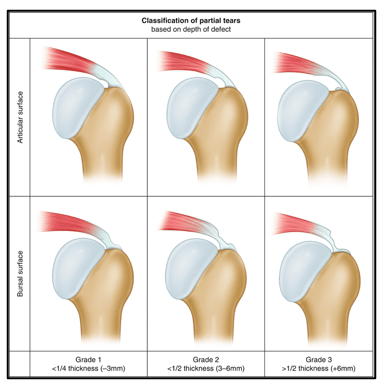
- Partial thickness tear: There is incomplete tearing of the tendon across its width. Some tendon fibres remain intact and are attached to the bone. There is no retraction of its torn tendon. The muscle still can do its intended actions.
These partial tears can be torn < 50 % or > 50 % across its width.
There are of 3 types of Partial Tears:
- Bursal surface partial tears: Occur on the superior (top) surface of the tendon, generally as a result of constant friction and impingement.
- Articular surface partial tears: Occur on the inferior portion (under-surface) of the tendon inside the joint. Commonly due to over-use or repeated sporting activities involving throwing actions.
- Intra-substance tears: This involves tearing of collagen fibres deep within the tendon substance of the rotator cuff. The superior and inferior surfaces of the tendon are intact. These tears are not visible during arthroscopy but are seen only on MRI films.
- Full Thickness Tears (Complete Tears)
The tendon tears completely across its full thickness (100 % of its width) and pulls away from its site of attachment on the upper humerus. The torn tendon is not able to perform its normal function of moving the humeral head (ball) and keeping it contained within the glenoid (shoulder socket).Over a period of time, this torn tendon retracts and the gap between its torn end and its original attachment site increases. The tears normally start off from the supraspinatus and can gradually spread to other tendons.
The common causes of a rotator cuff tear include:
An acute injury such as a traumatic fall or hard hit during athletic activities, or at work or an automobile accident. These traumatic tears may be associated with shoulder dislocations or fractures of the upper end of the humerus.
Chronic, continuous over-use that occurs with work-related activities or athletic training, such as baseball (pitching), or performing overhead movements in cricket, badminton tennis, swimming.
The gradual degeneration and aging of the muscles or tendons over time can cause a breakdown of collagen, thus making the tendons and muscles more prone to an injury.
About 30 % people above 60 years of age may have some form of rotator cuff tears. They may or may not have symptoms. With aging, there is reduction in the blood supply of the rotator cuff tendon. As a result, the tendons have a reduced ability for repair.
A torn rotator cuff is also associated with other shoulder conditions such as tendinitis and impingement. Surrounding bony structures can rub against the tendon surface and contribute to tendon fraying and tearing.
The symptoms of a rotator cuff tear can vary from patient to patient. They also depend upon the type of tear, location of the tear and the severity of any injury.
Common symptoms of rotator cuff tear are:
- Pain over the top of arm and shoulder. It may radiate towards the elbow.
- Inability to lift arm into overhead positions due to pain or weakness. Patients may also have difficulty in lowering their arm. This causes difficulties with routine daily activities like combing hair, changing dress or holding an object.
- Patients are unable to sleep on the affected shoulder due to pain
- Sleep gets disturbed due to associated tendon inflammation causing pain at night.
- Cracking or grinding sensation when trying to move the shoulder.
Pain of acute tear settles down over a period of time and movements along with function can return. But weakness continues to persist especially on stressing / loading of the shoulder.
The diagnosis of rotator cuff tears is based on the following:
- Careful history taking and clinical examination
- X-rays of shoulder joint – helps understand bony anatomy, quality of bones around the shoulder, presence of any bony spurs or arthritis of the joint.
- MRI Scan – provides information about the type of tear, quality of muscle and tendon, presence of retraction of torn tendon from its original footprint, any fatty atrophy of the muscle and presence of any bony spurs that may be pinching the tendon
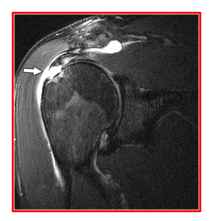
- USG Scan – Generally used in those patients who are not able to tolerate a MRI scan. Some doctors use this in OPD settings to diagnose rotator cuff tears.
The treatment for rotator cuff tears can be conservative (non-surgical) or surgical.
Non-Surgical Management of rotator cuff tears involves:
- Pain-killer and anti-inflammatory medicines
- Warm and cold fomentation – done 2 to 3 times a day
- Painkiller gel – used twice a day after fomentation to reduce muscle spasms and pain
- Physiotherapy – generally started after pain is brought under control first !
It helps in maintaining shoulder mobility, improving muscle strength and overall shoulder function.
- Steroid Injection – helps in reducing inflammation and controlling pain. Commonly a single shot is used. Repeated use of steroids can weaken the tendon and hence best avoided.
Such conservative (non-surgical) treatment is followed in older patients (> 65 years) having minimal pain, minimal weakness and good shoulder movements. It is also used when a patient has significant medical co-morbidities that would make the rotator cuff repair surgery risky.
Surgery for rotator cuff tears is indicated in the following circumstances:
- Acute full thickness (complete) rotator cuff tears with significant tendon retraction - such tears will not heal by themselves.
- Patients with full thickness tears who are suffering from significant pain, weakness and disturbed sleep.
- Partial rotator cuff tears that are more than 50% width of the tendon and also those smaller tendons tears (<50 % width) that do not respond well to non-surgical treatments.
The surgery of rotator cuff repair helps to heal the torn tendon, improve strength & mobility of the shoulder joint. This allows the shoulder to return to its pre-injury status.
Surgery is routinely performed by arthroscopic (key-hole surgery) or through mini-open techniques.
Compared to open surgery, arthroscopic rotator cuff repair is technically demanding. It needs specialised training and sophisticated equipment.
Dr Anand Jadhav does all his rotator cuff repair surgeries arthroscopically.
- Arthroscopic rotator cuff repair has following advantages:
- Tiny scars
- Minimal pain
- Shorter hospitalisation (day care or 1 day stay)
- Faster recovery
- Less wound complications
These are the steps involved in arthroscopic rotator cuff repair surgery:
- 3 to 4 Small skin incisions (portals) are made at pre-marked sites.
- Arthroscope (small telescope) is inserted and the joint is inspected thoroughly.
- Clearing of soft tissue debris, both inside and outside the joint, is done with specialised instruments. This assists in visualisation of all surrounding structures.
- Any thickened soft tissues (bursae) & bony projections (spurs/osteophytes) that may be pinching the top surface of the rotator cuff are cleared
- The torn tendon is identified, and its injury pattern and severity are noted. The tendon is checked for its mobility and ability to return to its original attachment site (tendon footprint) on the humerus.
- The site for tendon re-attachment is then cleared and roughened to encourage fresh bleeding that helps in tendon healing.
- Appropriate size suture anchors (metallic, non-metallic or soft tissue types) with attached strong non-absorbable sutures are inserted into the humerus, at appropriate locations, for allowing tendon repair. Then these suture ends are passed through the torn tendon with the help of specialised instruments.
- The tendon is mobilised, brought to its footprint with a grasper and held in its position for repair.
- The suture knots are tied securely without undue tension on the tendon edges. The repaired tendon is now at its desired location.
- The integrity of the repaired tendon is then checked thoroughly from inside the joint and also from the top surface.
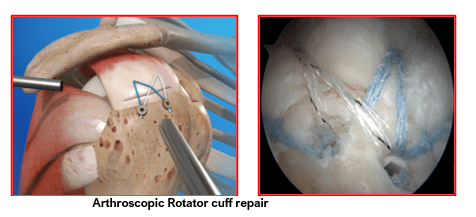
- Additional procedures may be needed and are commonly performed along with rotator cuff repair. These may include trimming of the bony spurs from the under surface of the acromion, trimming of downwards projecting osteophytes due to acromio-clavicular (AC) joint arthritis or fixing of a torn or displaced tendon of the long head of biceps (biceps tenodesis)
- At the end of the procedure, the repaired rotator cuff tendon should be able to move freely without rubbing against any bony surfaces and without lifting off from its repair site (footprint).
- The portal wound sites (incisions) are then closed with sutures or steri-strips (sticky tapes) and covered with sterile gauze and pressure paddings. These paddings help in soaking up the water that may leaks post-surgery.
- A shoulder sling (arm pouch) is applied. The patient is first shifted to recovery unit for 1 to 2 hours for close monitoring. After stabilisation the patient is then sent to his ward bed.
Patient’s expected progress after rotator cuff repair:
- Patients are allowed to start drinking water and eating food after 4 to 6 hours.
- They are given suitable pain-killer medicines as and when needed. These may be given as injections intra-venously or as tablets orally.
- Ice-packing to the shoulder is done about 4 to 5 times a day. The cold gel pads are applied for 15 to 20 minutes on each occasion. Ice packing needs to be carried on for 4 to 6 weeks post-surgery.
- Shoulder dressings are changed on the next day of surgery.
- Shoulder sling is worn for 4 to 6 weeks. It is permitted to be removed only for cleaning, bathing and doing shoulder exercises.
- Daily shoulder exercises are performed as instructed by an experienced physiotherapist. They need to be done at home twice a day before meals. These exercises are continued for the next 3 to 4 months in a progressive manner.
- Pain-killer medications are taken as required for first 2 weeks.
- Wound healing is confirmed, and any non-dissolving sutures removed at 10 days post-surgery.
It can take 6 to 12 weeks for healing of repaired rotator cuff tendon depending upon its size, quality of tendon tissue and type of repair performed. Recovery tends to be slower after cuff repair.
Patients need to be cautioned about the recovery time. A deliberately used GO SLOW regime works well in such patients in the long run.
It can take 3 to 4 months to regain full range of shoulder mobility. Sports specific training and strengthening of rotator cuff can be started at 3 to 4 months mark.
Unrestricted activities are generally permitted after 6 to 9 months.
An acute (recent) tear remains mobile and can be brought back to its original attachment site on the upper humerus. If the rotator cuff tears go untreated or get neglected, they become chronic tears.
The torn tendons get retracted and become weak. They are often scarred to the surround tissues and are immobile. They may not be in a position or state to be brought back to their original attachment sites. Surgical repairs are not possible in such chronic, retracted, immobile and severely weakened tendons. Their poor tissue quality cause sutures to cut through the tendon substance when trying to tie suture knots. Attempts to repair weak tendons are often abandoned.
Such patients often need some other forms of major treatments like shoulder tendon transfer or superior capsular reconstruction surgery if the joint is normal and non-arthritic.
In tendon transfer surgery, a healthy tendon is transferred and sutured to the defect within the rotator cuff tendon.
In the superior capsular reconstruction surgery, part of a flat body tissue (e.g. fascia lata from the thigh) is used as a patch to repair and augment the rotator cuff defect.
These surgeries allow the patients to get back some useful shoulder movements and functions, in addition to giving pain relief.
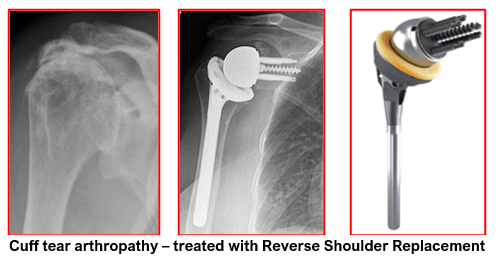
If the shoulder joint develops arthritic changes, secondary to the torn rotator cuff, it is called cuff tear arthropathy. In such cases a reverse shoulder replacement is advised.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

