Revision Total
Hip Replacement
Revision hip surgery or revision total hip replacement is a surgery where a surgeon removes the previous failed implants and replaces them with new implants. This surgery may involve the replacement of one or all of the components.
Revision hip replacement surgery is a complex procedure that requires extensive preoperative planning, specialized implants and tools, prolonged operating times, and an experienced surgeon having mastery of difficult surgical techniques, to achieve a good result.
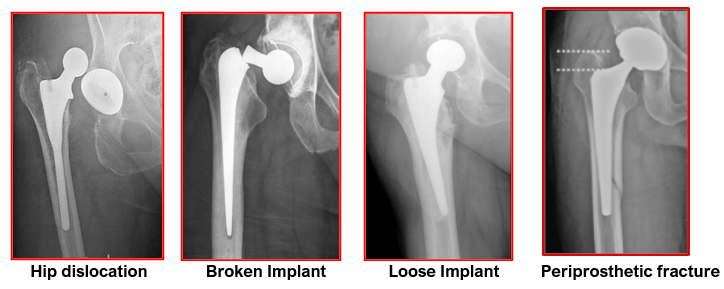
Revision Hip replacement surgery may be advised to patients if they have one or more of the following conditions:
- Loosening of the components in prosthetics that were originally cemented in place
- Wearing down of a prosthetic’s plastic components, causing an adverse reaction to the surrounding tissue
- Recurrent hip dislocations or instability
- Impingement and pain caused by improper placement of the prosthetic
- Fracture of the bone surrounding the prosthetic. Depending on the location and severity of the fracture, the surgeon may be able to fix it. If not, the prosthetic may need to be replaced.
- Fracture of the prosthesis itself. This needs removal and revision to a new prosthesis
- Adverse local tissue reaction caused by an outdated metal-on-metal implant that needs to be removed and replaced with a new prosthesis
- Infection in the bones or tissues near the prosthetic. This generally requires removing the infected prosthesis and curing the infection before implanting a new prosthetic
- Leg length inequality affecting quality of life.
Revision surgery may be needed soon after the original THR.
The following are reasons for short-term revisions: infection, recurrent hip dislocations, implant loosening from failed procedure, or a mechanical failure
Reasons for long-term revisions (i.e several years after the original THR): pain, loosening due to wear of mechanical components, late onset dislocations or peri-prosthetic fractures.
There are several mechanisms and reasons for failure of implants in a patient who has undergone hip replacement surgery.
Wear and Loosening: Properly functioning implants depend on their appropriate fixation to the bone. Firm fixation is usually achieved by cementing the implant into the bone. Some surgeons prefer biologic (non-cemented) fixation by using specially coated implants that allow bone growth to provide firm fixation and stability.
The firmly fixed implants, at initial hip replacement surgery, may become loose over time. Friction caused by the joint surfaces rubbing against each other wears away the surfaces of the implant and forms tiny particles that accumulate around the joint. In a process called aseptic (non-infected) loosening, the bond of the implant to the bone is destroyed by the body’s attempt to digest these wear particles. During this process, the normal bone is also digested which weakens or even fractures the bones. This condition is termed as osteolysis.
When the implants become loose, the patient may experience pain, change in leg length, difficulty in weightbearing or has hip dislocations due change in the alignments of the implants.
Aseptic loosening is the most common mode of failure of hip implants.
Infection: Infection is a serious and devastating complication of any surgical procedure. In total hip replacement, the large foreign metal and plastic or ceramic implants can serve as a surface for the bacteria to latch onto. They form a coating around themselves (biofilm) and become inaccessible to antibiotics. Even if the implants remain well fixed, the pain, swelling, and drainage from the infection make the revision surgery necessary. With current surgical techniques and antibiotic regimens, the risk of infection from total hip replacement is less than 1%.
Fractures: The location, type and extent of the fracture will determine if revision surgery is needed. Periprosthetic fractures (fractures around the hip implants) can occur due to trauma or repetitive stressing of the weak bones. This disrupts the implant fixation and makes them unstable of the implant which may warrant revision surgery. Rarely, the implant itself can fracture and needs revision surgery.
Instability / Dislocations: Instability occurs when the soft-tissue structures around the hip are unable to provide the stability necessary for adequate function during standing or walking. Instability may be the result of increased soft-tissue laxity (looseness), inadequate implant fixation, loosening of the implants and improper positioning or alignment of the prosthesis. Pain, instability or even repeated dislocations may alter the hip function and require revision surgery.
Patient-Related Factors: Patient’s age, activity levels, surgical history and weight can contribute to implant failure. Younger, more active patients have a higher rate of revision than older, less active patients. Obese patients have a higher incidence of wear and loosening. Patients with previous hip surgeries are also at higher risk for infection and implant failure.
After the decision for revision hip replacement is made, standard assessments are performed, including new long leg x-rays, blood tests, and possibly other imaging modalities like bone scan, CT scan or MRI scan.
X-rays may demonstrate a change in the position or condition of the components.
MRI helps to determine the cause, location, and the amount of bone loss before surgery.
Aspiration of the hip (joint fluid removed with a needle) may be required if infection is suspected. This aspirated fluid will then be sent to a laboratory for analysis to identify the specific type of organism causing infection.
- Most Revision Total Hip Replacements take longer to perform than the primary procedures (about two to three hours). It may involve the replacement of one or all of the components.
- The surgery is performed under long acting spinal, epidural or general anaesthesia.
- The surgeon makes an incision over the hip, preferably through the old scar, to expose the hip joint.
- Special retractors are used to keep the soft tissues apart. This allows good access to the hip joint and creates space for performing the revision surgery.
- The first step is removal of the failed implants. The old femoral component of the hip prosthesis is removed first using special cutting devices and extractors. In a well cemented or well-fixed uncemented femoral stem there is need to perform an extended femoral osteotomy (ETO). The femur bone is cut widely to open its canal and remove a well-fixed implant and any cement mantle. After removing the implant and any cement mantle, the femur is fixed and held together with 3 to 4 metallic encircling wires and special cables.
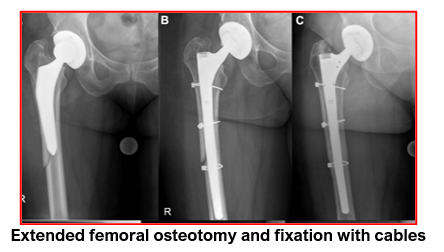
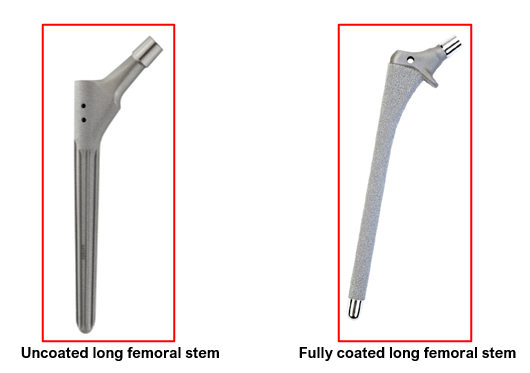
- The femur then is prepared to receive its new prosthesis. In some cases, the damaged bone gets removed. Hence bone grafts and special wire mesh may be used to reconstruct the lost proximal bone and strengthen the femur. In extensive bone loss cases, specially coated metallic cones may be used for reconstruction of the upper femur. Additionally, long length femoral stems need to be used for providing extra fixation to the implant and stability to the hip joint.
- Then the acetabular liner and its cup (i.e the outer shell of uncemented acetabular implant) are removed. In cemented acetabular implants, the plastic cup is removed along with the mantle of underlying cement.
- In either scenario, the acetabulum is cleaned and assessed for the amount of bone loss after implant removal. It is then prepared to receive its new prosthesis. Depending upon the shape of the acetabulum and the amount of bone loss, cemented or uncemented acetabular cups are used. In situations with extensive bone loss, there is need for using bone grafts, special acetabular metal cages and screws to reconstruct and strengthen the acetabulum. Then an appropriate size plastic cup in inserted with bone cement.

- In cases with minimal bone loss, uncemented implants are considered good for use if firm hold (tight fit) is confirmed on trial implants. Appropriate size acetabular liner and femoral implants, without cement, are attached to the bones. Then a trial plastic head, of sufficient height and diameter, is used to provide a stable joint. After all trials are in place, range of hip motion, hip stability and leg lengths are confirmed. After this confirmation, all trial implants are removed.
- The femoral and acetabular bones are thoroughly washed out and dried in preparation for using cemented implants as per the trial sizes. Standard cementing and prothesis implantation techniques are used for both the acetabulum and the long stem femur.
- If using uncemented acetabular implants (without cement), additional fixation techniques like screws for the cup shell are used for locking the implant firmly to the underlying native acetabulum. The new plastic or ceramic liner of correct size is firmly attached to the uncemented acetabular cup. The acetabular side work is always completed first before implantation of the femoral prosthesis.
- If using uncemented femoral implant, a long stem implant is inserted. This implant may be uncoated, partially coated at upper end or fully coated along its full length. This coating encourages bony ingrowth and provides additional stability to the implant.
- The correct diameter ball (femoral head) with appropriate neck length is attached to the top of the femoral stem.
- The acetabular and femoral implants are then brought together to form the new joint. The new hip is moved for re-testing joint stability, range of movements and leg lengths.
- As the bony deformities can be of any type, the operating surgeon needs to have all types of acetabular and femoral implants and other inventory ready in the operation theatre. Such planning enables him to use the most appropriate revision implants and ensure the best possible outcome for the patient.
- At the end of the surgery, the joint is thoroughly washed out, any bleeding points are secured and sealed with cautery to avoid bleeding.
- The wound is then closed in layers after keeping a suction drain inside to drain out excess blood from the hip joint.
- Sterile dressing and compression bandage are applied. Patients are also provided with a triangular foam (abduction wedge) to keep their legs apart and to avoid crossing over each other. This helps in preventing hip dislocations whilst the tissues are healing.
Post-operative care after hip revision surgery is very similar to the care of a primary hip replacement. This includes a combination of pain medication and blood management as necessary. Physiotherapy is started after few hours post-surgery to encourage ankle and toe movements. Appropriate antibiotics and some method of blood clot prevention (DVT Prophylaxis) will be continued in the postoperative period. Abduction wedge is used for minimum 6 weeks post-surgery to keep legs apart.
In most cases, physiotherapy will be initiated within 24 hours of the procedure. Full Weight Bearing (FWB), Partial Weight Bearing (PWB) or Toe Touch Weight Bearing (TTWB) is used as per surgical findings and complexity of the procedure. Therapy will usually continue for up to three months following the surgery. Assistive devices, such as a walker or crutches, will be used early in the post-surgery phase, and patients will progress to a stick or unaided walking as their condition and confidence improves.
Patient’s hospital stay can be between 3 to 5 days depending upon the complexity of the case.
Recovery time after revision hip surgery is variable depending upon several factors. Post-surgery rehab plans need to be individualised based on these variable factors. Patients should be forewarned about this recovery duration.
Any surgery can have potential complications. The complexity of revision joint surgery increases the chance of surgical complications which are similar to the primary THR.
Possible complications include:
- Infection
- Bleeding
- Damage to nerves or blood vessels
- Intra-operative fractures – occur during removal of the old implants or the insertion of new ones.
- DVT (Deep Venous Thrombosis) or blood clots
- PE (Pulmonary Embolism)
- Implant loosening, especially in overweight patients
- Dislocation of the new implants. (Higher compared to primary THR).
- Difference in leg length resulting from shortening or lengthening of the leg with the new prosthesis
- Formation of heterotopic bone, which is bone that develops at the upper end of the femur following surgery. (Joint infections after surgery increase risk for this)
Infection, bleeding, damage to nerves or blood vessels, and intra-operative fractures can be minimized by using antibiotics before and after surgery, sterile surgical techniques and utilizing well-planned surgical exposures.
Similar to primary THR, some mild swelling of the leg may be present after surgery for as long as 3 to 6 months. Swelling can be treated by elevating the leg, applying an ice pack, and wearing compression stockings.
Pre-existing medical conditions, such as heart and lung complications, or stroke conditions, can be aggravated by a revision procedure. These conditions may also develop in patients after revision surgery. Very rarely, death can occur. The decision to perform revision joint surgery is made when the benefits of pain relief and functional improvement outweigh the risk of potential complications.
The benefits of PSI technology for Total Knee Replacement are significant in terms of optimised patient outcomes, safety and healthcare economics.
- Use of advanced software that allows 3D reconstruction of the joint and supports all
implant sizes
- The restoration of the mechanical axis
- Special consideration given to the rotational alignment of the tibial tray
- Optimised patella tracking
- Personalised posterior slope
- Restoration of the joint kinematics
- Disposable instrumentation
- Minimised risk of cross contamination
- Instrument sterilisation & processing costs are saved
- Replacement / refurbished instrumentation not needed saving costs
Total hip replacement (THR) surgery is a very is a common surgery performed for advanced hip arthritis. It gives significant improvements in hip pain, mobility, function and quality of life. Outcomes following THR are generally excellent in the majority of the patients.
Infection after THR is rare and occurs in less than 1 % of patients undergoing primary THR. But it remains a challenging problem that can be difficult to diagnose and treat.
A THR may become infected due to the presence of bacteria around the hip soft tissues, the artificial implants and the underlying bones. This can lead to bone destruction, implant loosening, deformity of the affected leg and poor quality of life due to pain and reduced mobility.
Infection can set in during the time of surgery, or anywhere from weeks to years after the surgery.
The most common ways for harmful bacteria to enter the body and cause the infection are:
- Through the surgical incision made for the THR or through any breaks or cuts in the skin
- During major dental procedures (such as a tooth extraction or root canal). Bacteria get carried to the knee via the bloodstream.
- Through wounds from other surgical procedures
After reaching a person’s new artificial hip joint, the bacteria may multiply and cause an infection.
Some bacteria are harmless, such as those that occur naturally in the stomach, while others may harm a person and cause an infection. A person’s immune system usually kills any harmful bacteria that get into the bloodstream. When a person has a hip replacement, their hip joint is replaced with an artificial joint made of metal and plastic/ceramic. These materials are not organic and hence it is harder for the body to kill the bacteria stuck on them.
Anyone who has a hip replacement can develop an infection after surgery, but some groups are at a greater risk of infection. These include people who:
- have immune deficiencies, such as HIV or lymphoma
- have diabetes
- have poor circulation in their hands or feet
- are using treatments that suppress the immune system, such as chemotherapy or corticosteroids
- have frequent urinary tract infections
- have a BMI of over 50
- have dental problems
- have dermatitis or psoriasis
- have rheumatoid arthritis
- smoke or chew tobacco
- have undergone hip surgery previously
- have had an infected THR previously
The THR infection may be superficial during the early phase of 2 to 4 weeks post-surgery and be limited to the subcutaneous tissues only without any breach of the deep fascia.
If the infection breaches the deep fascia and goes deeper, it becomes a deep infection. This can generally happen 4 to 6 weeks after surgery. It involves the deeper tissues and also spreads around the implants used for replacing the hip joint. It can go onto involve the underlying bones as well.
The symptoms and signs of infection after THR are:
- Increased pain or stiffness in a previously well-functioning hip joint
- Difficulty in walking and weight bearing
- Swelling around the hip region
- Warmth and redness around the hip wound
- Wound drainage
- Fevers, chills and night sweats
- Fatigue
- Patient may be walking with a limp
- Deformity of the leg with limb length inequality
- Presence of any wounds (sinuses) with or without discharge
- Hip may be tender and have painfully limited knee movements
Infection after THR is based on patient’s complaints, his physical examination,
X-rays, blood tests, MRI or CT scan, Bone scan and hip joint fluid aspiration.
Specific blood tests can help identify an infection. 3 blood tests are routinely performed for patients with suspected infection of TKR – Haemogram (complete blood cell count – CBC), Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP). Haemogram helps to monitor the white cell count. The ESR and CRP tests measure the level of inflammation in the patient’s body. Although neither test will confirm the presence of infection, if either or both of them are elevated, it raises the suspicion that an infection may be present. If the results of these tests are normal, it is unlikely that the patient’s joint is infected.
Aspirated fluid from the hip joint can help identify an infection. Under strict sterile conditions and with proper aseptic precautions, a needle to inserted to draw fluid from the hip joint. An image intensifier may be used to confirm position of needle within the hip joint before aspiration of the fluid. This fluid is sent to the laboratory for examination under microscope for presence of any micro-organisms. The samples are also cultivated and monitored to see if any bacteria or fungus grow from the fluid.
The joint fluid is also analyzed for the presence of white blood cells. In normal hip fluid, there are a low number of white blood cells. The presence of a large number of white blood cells (particularly cells called neutrophils) indicates that the joint may be infected. The fluid may also be tested for specific proteins that are known to be present in the setting of an infection.
The treatment options available for managing an infected THR patient are:
Non-surgical (conservative) and Surgical Treatments.
Non-surgical (conservative) Treatment: useful in a limited group of patients who have superficial infection. The skin or the subcutaneous layers are involved without involvement of the deep fascia or underlying deeper tissues or the artificial joint implants. Such cases need to be diagnosed quickly and their treatment started as soon as possible. This involves administration of intra-venous or oral antibiotics for 5 to 7 days. Early treatment in such patients with superficial infection helps in controlling the infection and allows healing with good success rate.
Surgical treatment: is invariably needed for patients presenting late and in those patients in whom the infection has now involved the deeper tissues and also the hip implants.
There are two types of surgeries commonly performed for managing an infected THR.
Hip Debridement – This procedure involves surgical washout of the joint. It is done for deep infections in a THR that are picked early (within several days of their onset), and those that occur within weeks of the original surgery. This can be within first 2 to 4 weeks post-surgery. Deep infections that are caught very early, may sometimes be cured with joint debridement.
During this procedure, the surgeon reopens the surgical wound to gain access to the hip joint and removes all contaminated soft tissues. Fluid and tissue samples are collected to confirm presence and type of micro-organisms causing the infection. The metallic implants are thoroughly cleaned with sterile normal saline, and the plastic liner of the uncemented acetabular cup is exchanged for a new plastic liner. The femoral head implant is also exchanged. The wound is then closed in the usual manner over a deep wound drain that gets removed after 24 to 48 hours. Patients are given suitable intravenous (IV) antibiotics for approximately 6 weeks. These need to be changed or continued as per antibiotic sensitivity reports from the labs.
Staged surgery:
Infections that have been present for longer periods of time (more than 6 weeks) and Late infections (those that occur months to years after the joint replacement surgery), almost always, requires a two staged surgical plan.
In general, the longer the infection has been present, the harder it is to cure without removing the implant. The bacteria adhere to the implants and form an impregnable biofilm layer around themselves. The biofilm does not allow any antibiotics to reach the bacteria. The biofilm is also difficult to be scrubbed off the implants and the underlying bones. Hence complete implant removal remains the best option to control infection.
The FIRST STAGE SURGERY includes:
- Removal of the artificial joint – This is done with help of specialised instruments whilst taking care to avoid damage to the underlying bones and maintain the bone stock.
- Extended femoral osteotomy (ETO) may be needed in cases where the femoral implant (cemented or uncemented) is firmly fixed within the femur.
- Soft tissue debridement and Joint washout – helps get rid of infected soft tissue in the joint.
- Placement of antibiotic spacer – Spacers are made with bone cement that is loaded with antibiotics. These are prepared on table with special moulds or can be shaped by hand to fill the acetabulum and femur. The spacers help to maintain the joint space, prevent soft tissue scarring and keep the joint aligned while the infection is being treated. Specialised articulating spacers also allow hip movements and weight bearing. The antibiotics from the cement spacer flow into the joint and surrounding tissues and, over time, help to eliminate the infection.
- Antibiotic Therapy – Patients who undergo staged surgery typically need at least 6 weeks of IV antibiotics, or possibly more, before a new joint replacement can be implanted. Orthopaedic surgeons work closely with their microbiology colleagues, for their help and guidance, in choosing the right and most effective antibiotic, best method of its administration (oral or intravenous) and the duration of the antibiotic therapy.
- Serial blood tests are done for monitoring the response to the antibiotics and also to note if any untoward side-effects are occurring in the body.
Normally 6 weeks of antibiotics are given intra-venously.
SECOND STAGE SURGERY:
This stage involves the insertion of new hip replacement implants
It is generally performed 6 weeks after the first stage. The blood counts have to be satisfactory and normal. This indicates that the joint infection has come under control. Patient should also be optimally fit to undergo this second stage.
The hip joint is exposed, the spacers are removed, the joint is debrided and washed out. The bones are prepared to receive the new implants.
The acetabulum may need use of special cages if there is bone loss on the acetabular side. New plastic cup in inserted with bone cement in such cases.
If it is possible to insert a tight-fitting acetabular cup during trial, then specially coated uncemented cup is inserted and secured with 2 screws. Then a plastic or ceramic liner is inserted as per pre-op plans.
On the femoral side, long stem uncemented implants are more popular in use. They provide fixation at lower end of the femur bone. This wide zone of fixation provides good stability to the femoral implant. These long stem implants can be used even with loss of bone at upper femur region as they rely on fixation at lower femur and not the upper femur.
Appropriate diameter ball (femoral head) with correct neck length (as per trialing) is placed and secured atop the long stem uncemented femoral implant. Then the new joint is relocated. Hip range of motion, stability and leg lengths are re-confirmed.
Wounds are closed in the standard manner over a deep drain in the hip. This gets removed after 24 to 48 hours. An abduction wedge is placed between the leg to avoid risk of dislocation if legs cross over.
SINGLE STAGE REVISION SURGERY: During this single staged surgery, the implants are removed, the joint is thoroughly debrided (including the soft tissues and bones), the bones are reshaped and prepared to take the new implants. The new implants are inserted as usual, all in a single stage. The wounds are closed over a drain as usual.
Single-stage surgery is still not as popular as the two-stage surgery. But it is gaining wider acceptance as a method for treating infected total joints. It is more popular in Europe (especially, Germany). Surgeons are still observing the studies and outcomes of single stage revision joint replacements.
The following steps and precautions may help in reducing the risk of infection in a patient undergoing hip replacement surgery:
- Using prophylactic antibiotics: Preventive medicines may help reduce the risk of hip replacement infection. We usually give three doses of intra-venous antibiotics within first 24 hours with the first dose given 20 to 30 minutes before skin incision is taken.
After their THR, patients may also need prophylactic antibiotics for other surgeries like dental work.
- Keeping operation time short: Surgeon should be experienced and sleek in his surgery to keep the operating time short. This helps to reduces the length of time the wound is open and vulnerable to infection.
- Reducing the number of people present: Limiting the number of people and limiting the number of times, they come and go may reduce the bacterial counts in the room and decrease the risk of infection.
- Using sterile equipment: The operation theatre and surgical instruments should all be thoroughly sterilized. The instruments should not be exposed to any contamination. The implants used during surgery should be in pre-sterilised airtight packages. Before using them, their sterility should be confirmed and maintained throughout the surgery. All staff involved in the joint replacement surgery must use disposable drapes and surgeon gowns. They must change gloves frequently as needed during the surgery.
- Screening for bacteria in the nose: If a person has certain types of harmful bacteria in their nasal passage, they may increase the risk of infection. Some hospitals screen for these bacteria before operating. If harmful bacteria are found, the person will be given an antibacterial ointment to use. Some hospitals will routinely decolonize nasal passages with mupirocin several days before surgery.
- Washing with chlorhexidine: This may help reduce the number of harmful bacteria on the skin before surgery.
- Thorough skin cleaning in OT: The operative leg including foot must be thoroughly cleaned before surgical preparations. This also helps to control risk of infection.
- Having standardised protocols: Wards and OTs for joint replacement surgeries should follow standard protocols which help in maintaining discipline from all concerned staff and bring in uniformity in precautions to be taken during hip replacement surgeries.
After a THR, following measures may help reduce the risk of infection:
- Following the surgeon’s advice on how to treat the wound
- Clean and cover cuts, wounds, or burns as soon as they happen
Maintain dental hygiene, as infections in the mouth may spread to the artificial joint
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

