PCL Injuries & Management
The posterior cruciate ligament (PCL) is one of the main restraining ligaments of the knee. The PCL is situated in the centre of the knee and runs from the back of the tibia to the front of the femur. PCL is thicker and stronger than the ACL or other ligaments of the knee.
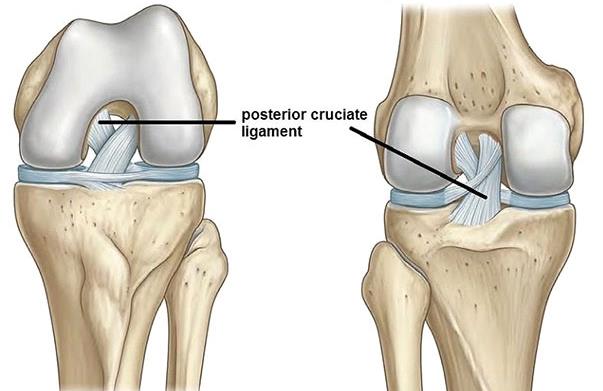
The PCL acts to prevent excessive backward movement of the tibia. It keeps the knee stable, along with other knee ligaments, during rotational movements like twisting, turning or side-stepping activities.
Another important function of the PCL is to provide important neurological feedback about orientation of one’s limbs in space. This perception is important for normal joint function in daily activities, occupational tasks and sports.
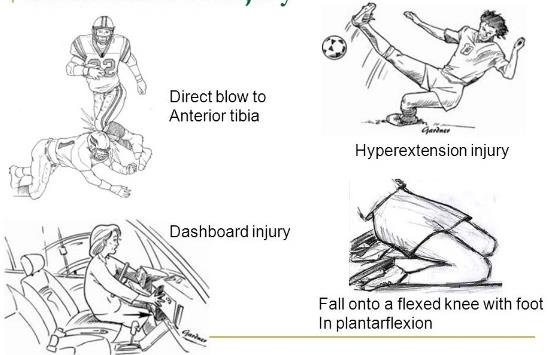
An injury to the posterior cruciate ligament (PCL) can happen in many ways. Being a thick and strong ligament, a powerful force is needed to injure the PCL. PCL injuries are less common compared to the anterior cruciate ligament (ACL).
Some of the common causes of PCL injuries are:
- Motor vehicle accidents – A direct blow to the front of the knee such as a bent knee hitting a dashboard in a car crash (dashboard injury) or a fall onto a bent knee from a motorbike. The tibia is forced backwards injuring the PCL.
- Contact Sports: Athletes in sports, such as football and rugby, can tear their posterior cruciate ligament when they fall on a bent knee with their foot pointed down. The tibia hits the ground first and it moves backward. Being tackled when your knee is bent also can cause this injury.
- Knee twisting or Hyperextension: can cause pulling or stretching of the PCL
- Simple misstep: can cause a person to fall and his tibia to hit against the edge of a step. This forces the tibia backwards and the PCL gets injured.
Meniscal injuries: either the outer (lateral) meniscus or inner (medial) meniscus or both can be injured.
Cartilage injuries: The articular cartilage lining the femur, tibia or patella could be damaged. These cartilage lesions could be from minor flaps to major defects.
Ligament injuries: Medial collateral (MCL), lateral collateral (LCL) or Anterior cruciate ligament (ACL) injuries may also occur.
Fractures: could involve the tibia, femur or patella.
The typical symptoms of a posterior cruciate ligament acute injury are:
- Pain with swelling that occurs steadily and quickly after the injury
- Swelling that makes the knee stiff and may cause a limp
- Difficulty in walking
- The knee feels unstable, like it may “give out”
If there are no associated injuries to other parts of the knee, the signs and symptoms of a posterior cruciate ligament injury can be so mild that the patient might not notice that anything is wrong with their knee. Over time, the pain gets worse and the patient’s knee feels more unstable. They may have difficulty with kneeling or stair climbing.
If other parts of patient’s knee have also been injured, then his signs and symptoms will likely be more severe.
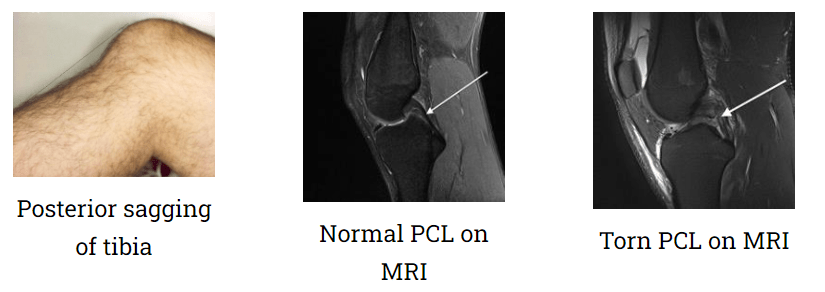
PCL injury is diagnosed based on patient’s history of injury, symptoms, thorough clinical examination and investigations like X-rays and MRI of the knee. Special tests for PCL confirm excessive backward movement of tibia over the femur (posterior sagging).
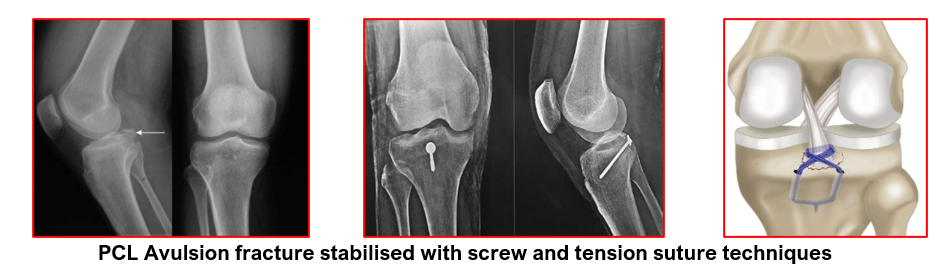
A torn PCL is not seen on x-rays. But an x-ray may show posterior sagging of the tibia and also any fractures of the upper tibia where PCL is normally attached (avulsion fractures).
MRI scan of the knee can clearly show a posterior cruciate ligament tear and determine if other knee ligaments or cartilage also are injured. It can also show bony bruises and also fractures which may not be very obvious on the x-rays
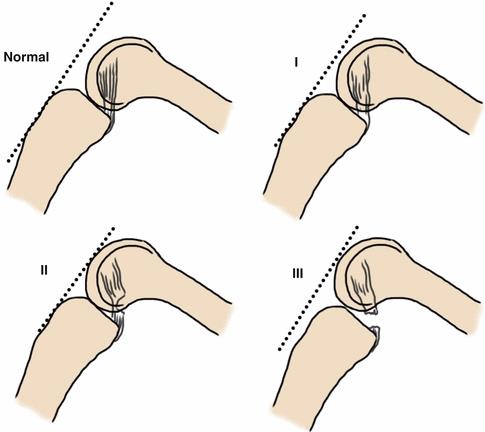
PCL injuries are traditionally classified into 3 grades as follows:
Grade I (Mild) — A mild injury causes only microscopic tears (sprain) in the ligament.These tiny tears can stretch the PCL out of shape, but it still retains the ability to stabilise the knee.
Grade II (Moderate) — The PCL is partially torn, and the knee is somewhat unstable, meaning it gives out periodically when you stand, walk or have diagnostic tests.
Grade III (Severe) — The PCL is either completely torn or is separated at its end from the bone that it normally anchors to. The knee is more unstable. Because it usually takes a large amount of force to cause a severe PCL injury, patients with Grade III PCL injuries often also have sprains of the ACL or collateral ligaments or other significant knee injuries.
The most common types of PCL injuries are Grade I & II — small sprains and partial tears. The grade of PCL injury and patient’s symptoms help in deciding the right course of treatment for the patient.
Not all patients with PCL injury need surgery. You may choose not to have surgery if you:
- Have a minor tear in your PCL (a Grade I or II tear that can heal with rest and rehabilitation) or have a chronic PCL tear without any symptoms.
- Are not very active in sports and your work does not require a stable knee.
- Are willing to stop doing activities that require a stable knee or stop doing them at the same level of intensity. You may choose to substitute other activities that don’t require a stable knee, such as cycling or swimming.
- Can complete a rehabilitation program that stabilizes your knee and strengthens your leg muscles to reduce the chances that you will injure your knee again and are willing to live with a small amount of knee instability.
- Do not feel motivated to complete the long and rigorous rehabilitation program necessary after surgery.
Conservative treatment for PCL injuries is generally used for all grade of PCL injuries in the initial phase. This can be the definitive treatment for Grade I or Grade II injuries:
- Rest– from sports or heavy work
- Ice pack– to reduce swelling and pain. Done for 15-20 minutes on each occasion for 3-4 times daily.
- Anti-inflammatory medications– reduce pain and inflammation. They allow patients to tolerate physiotherapy
- Physiotherapy – all muscles around the knee must be strengthened especially the Quadriceps. These muscles can then take over some of the PCL’s role in knee stability. As the PCL has an important role in providing information to the muscles and brain about the position of the knee joint (balance and proprioception) specific re-training of other nerves is performed to help compensate.
- Functional Knee Braces – are prescribed to help patients with damaged PCLs. They provide support and stability to the knee joint whilst allowing healing of the PCL. They also allow controlled range of knee motion exercises and help with knee proprioception. A pillow is kept under the calf to prevent posterior sagging of the tibia whilst the PCL injury is healing.
PCL reconstruction is recommended when you:
- Have completely torn your PCL (Grade III injury) or have a partial tear and your knee is very unstable.
- Have injured other parts of your knee, such as the articular cartilage, meniscus, other knee ligaments or have fractures.
- Have a displaced avulsion fracture of the upper tibia (PCL avulsion fracture)
- Are very active in sports or have a job that requires knee strength and stability (such as construction work), and you want your knee to be as strong and stable as it was before your injury.
- Are willing to complete a long and rigorous rehabilitation program.
- Have chronic PCL deficiency that is affecting your quality of life.
Have gone through a rehabilitation program and your knee is still unstable.
PCL surgery can either be a Reconstruction surgery for a torn PCL or a Fracture fixation surgery for a PCL avulsion fracture.
A knee with completely torn PCL or an avulsed upper tibial fracture, with attached posterior cruciate ligament (PCL avulsion fracture), has abnormal mobility of the tibia during normal activities and sports. These patients have continued instability, pain, swelling and inability to lead an active lifestyle. If these types of injuries are not treated properly or if they get neglected, they can cause secondary damage to the joint cartilage and the meniscal tissues leading to knee arthritis at a younger age.
PCL surgery is recommended as it helps to:
- restore normal or almost normal stability in the knee
- return you to the level of function you had before the knee injury
- limit loss of function in your knee
- prevent injuries to other knee structures and
- prevent early knee degeneration.
- lead an active lifestyle
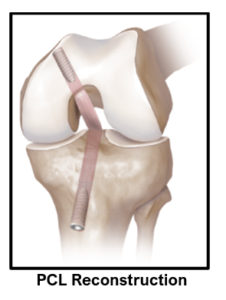
PCL reconstruction is a surgical procedure to replace the stabilizing function of the posterior cruciate ligament.
It involves removing the remains of the damaged PCL and replacing it with another form of soft tissue, called a graft.
A number of grafts are available for use to reconstruct the PCL. The two commonest grafting techniques are to use the hamstring tendons (the semitendinosus and gracilis tendons) or a so called BTB (bone tendon bone) graft. The BTB graft has a bony plug from the patella at the top, the patellar tendon tissue strip in the middle and another bony plug from the upper tibia at the lower end.
PCL reconstruction surgery is done arthroscopically (through key holes) using telescope, camera and specialized instruments.
Dr Anand Jadhav performs all PCL surgeries arthroscopically because it offers:
- Excellent visualization of structures in the knee joint
- Tiny scars offer better cosmetic results
- Minimal tissue damage and bleeding
- Less pain
- Early rehabilitation
- Short hospitalisation
There is a 90 to 95% chance of a good result in patients who are having the operation for appropriate reasons and who comply with post-surgery PCL rehabilitation (6-9 months). These patients have good muscle strength, knee stability and a painless range of motion. Patients can return to their pre-injury occupation or sports.
The steps of a standard PCL reconstruction are:
- PCL reconstruction surgery is done under general, spinal or epidural anaesthesia.
- A tourniquet is applied on the upper thigh in order to provide bloodless operating field.
- Diagnostic arthroscopy is performed through two tiny keyholes (portals) on either side of lower portion of knee cap.
- Any meniscal or cartilage injuries are dealt with. Additional portals (posteromedial and posterolateral portals) are made as needed on the back sides of the knee to complete the joint examination and help in preparation for further surgical steps.
- The remnants of the torn PCL (stumps) are cleared with a shaver from the femur and tibia.
- Sites for inserting new PCL at tibial and femoral ends are clearly identified and marked.
- Hamstring tendon grafts (semi-tendinosis and gracilis) are harvested through a small incision on upper part of leg. The graft is prepared in a manner so as to make it as thick as possible and also maintain sufficient length.
- Alternatively, a bone tendon bone (BTB) /patellar tendon bone (PTB) graft can be harvested from the patella and upper tibia along with a strip of patellar tendon. It is then prepared for grafting.
- The graft diameter and length are noted down after graft preparation.
- Tibial and femoral bone tunnels of matching diameters and desired lengths are then drilled with help of special guides.
- The hamstring / BTB graft in now pulled into the knee joint through the tibial tunnel and then further upwards through the femoral tunnel.
- The femur side graft fixation is done either with an endo-button (a suspension device) or a metallic or absorbable screw.
- The graft is then tensioned with a special device to remove any slack within the graft.
- The tibial side fixation is done with an appropriate implant (metallic /absorbable screw or a suture disc) whilst holding the tibia in its normal position by manually correcting its posterior sag and keeping the graft under tension.
- The new PCL is now checked arthroscopically for its position, tension, fixation strength and any signs of impingement against any part of the knee.
- The portal wounds are closed, and dressing pads are applied. A compression bandage is given.
- A hinged PCL knee brace, locked in 0 degrees extension, is also applied.
After your PCL surgery, my team will guide you through your recovery period.
- Hospital stay is for 1-2 days only. Patients can start moving their toes and ankles as soon as their anaesthesia wares off. Water and food intake can be started after 2 to 3 hours post-surgery. Suitable painkiller medications are given either intra-venously or orally.
- Walking can be started on the same day or the next day of the surgery. The patient usually needs the help of elbow crutches or a walker for mobilisation. Further support of the elbow crutches may be needed for a period of 2 to 6 weeks depending on patient’s progress.
- Regular ice packing is done 3 to 4 times a day and carried on for 4 to 6 weeks after discharge.
- Patients are allowed to fully weight bear with their knee brace locked in extension at 0 degrees and used like this for the first 2 weeks. The knee brace is then set to allow 90 degrees of knee flexion (bending) after 2 weeks. After 6 weeks, full knee flexion is allowed as tolerated. The knee brace is needed for 3 months in total.
- Patients are advised to keep a pillow under the calf of the operated leg to avoid posterior sagging of the tibia and stretching of the new ligament. This is carried on for 3 months.
- They are also given instructions about the type of exercises to be done and are encouraged to continue their rehabilitation further for 6-9 months in a stepwise manner to gain maximum benefits from the PCL reconstruction. These exercises will be monitored weekly by our physiotherapist for the first 3 months.
- I recommend that you continue physiotherapy for a minimum of 3 months to regain normal range of knee motion, good muscle strength and sense of stability (proprioception) in the knee joint. Patients who comply with PCL rehabilitation have a very high chance of a good result. Stability is restored and they can undertake most of the normal activities, including sports.
- Office type work can be resumed after 2 weeks provided transport is arranged. You can drive a car after 4-6 weeks and ride a motorbike after 6-8 weeks provided your knee is reasonably pain-free with good range of motion, strength and stability. Heavy-duty work can be started after 3 months.
- Generally, any sort of sporting activity is restricted for first 6-9 months. During this period, knee exercises, weight training and sports specific training are carried on. Full intensity sports are allowed after 9 months of rehabilitation.
PCL avulsion fractures can be treated conservatively or surgically depending on the size of the fragment, amount of displacement, age and activities of the patients.
Un-displaced PCL avulsion fractures are treated conservatively in a PCL knee brace for 3 months. But these types of fractures need serial x-rays for the first 4 weeks to ensure that the fragment is stable in its place without getting displaced and is showing signs of healing. Knee flexion (bending) can be started gradually with support of the brace after 4 weeks. A pillow is used under the calf to avoid posterior sagging of the tibia.
Displaced PCL avulsion fractures can be treated arthroscopically if fragment is small sized. Specialised sutures are tied around the avulsed fragment arthroscopically and brought out in the front through drill holes in the upper tibia. After x-ray confirmation of proper fracture reduction, the fracture fragment is secured to the upper tibia by tying suture knots over a suture disc or through additional drill holes in the upper tibia. The PCL is checked for its stability and tension post-fixation.
If the fracture fragment with attached PCL is large in size, then an open posteromedial approach is used to reduce the fracture fragment under direct vision and fixed to the upper tibia with screws and washers. Knee x-rays are taken for confirmation of accurate reduction and stable fixation.
The patient is given a PCL knee brace. They are allowed to mobilise non-weight bearing with crutches for first 4 weeks. Full weight bearing is started after 1 month. Knee flexion is started at 2 to 3 weeks after confirming with knee x-rays that there is no displacement of the fixed fracture fragment. Knee range of motion is allowed freely in the knee brace after 1 month. Brace is needed for 3 months.
X-rays are done at 4, 8 and 12 weeks after surgery to assess fracture healing. Further rehab is like in a standard PCL reconstruction.
Most athletes with PCL injuries, who are treated without surgery, return to their sport at their pre-injury activity level after appropriate rehabilitation.
Most patients, who have undergone surgical reconstruction of the PCL, are able to return to their pre-injury level of physical activity within 1 year after surgery.
As a long-term complication, many (but not all) patients with PCL injuries eventually develop osteoarthritis in the injured knee joint. On average, the arthritis symptoms begin 15 to 20 years after the initial PCL injury.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

