Patello-Femoral Instability
The knee can be divided into three compartments: patella-femoral, medial and lateral compartment. The patella-femoral compartment is the compartment in the front of the knee between the patella (kneecap) and the lower femur (thigh bone).
The medial compartment is the area on the inside portion of the knee, and the lateral compartment is the area on the outside portion of the knee joint.
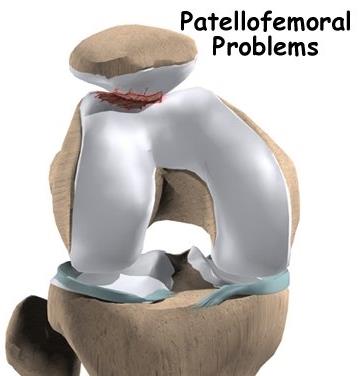
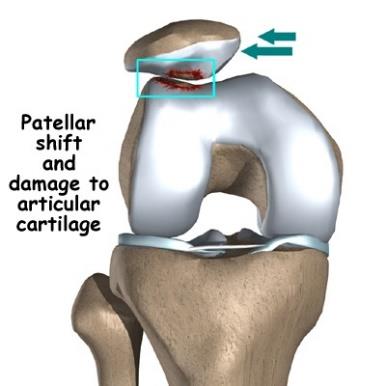
Patellofemoral instability means that the patella (kneecap) moves out of its normal pattern of alignment. This malalignment can damage the underlying soft structures such as muscles and ligaments that hold the knee in place and also the articular cartilage of the patella and femoral trochlea.
Patello-femoral instability can be caused because of variations in the shape of the patella or its trochlear groove as the knee bends and straightens. Normally, the patella moves up and down within the trochlear groove when the knee is flexed or extended. Patello-femoral instability occurs when the patella moves either partially (subluxation) or completely (dislocation) out of the trochlear groove.
A combination of factors can cause this abnormal tracking and include the following:
Anatomical defect – Flat feet or fallen arches and congenital abnormalities in the shape of the patella bone or the femoral trochlea can cause misalignment of the knee joint.
Abnormal Q angle –The high Q angle (angle between the hips and knees) often results in mal tracking of the patella such as in patients with knock knees.
Patellofemoral arthritis- Abnormal tracking of the patella at the patellofemoral joint can eventually lead to loss of the articular cartilage on the back of the patella and consequent patellofemoral arthritis.
Improper muscle balance- Weak quadriceps (anterior thigh muscles) can lead to abnormal tracking of the patella, causing it subluxate or dislocate laterally.
Young active individuals involved in sports activities are more prone to patellofemoral instability.
Patellofemoral instability causes pain when standing up from a sitting position and a feeling that the knee may buckle or give way. When the kneecap slips partially or completely you may have severe pain, swelling, bruising, visible deformity and loss of function of the knee. You may also have sensational changes such as numbness or even partial paralysis below the dislocation as a result of pressure on nerves and blood vessels.
The diagnosis of patellofemoral instability is made based on patient’s medical history, thorough clinical examination and appropriate investigations.
Knee X-rays in 3 different planes show the position of the patellofemoral joint, changes in patellar position or tilt, patellar subluxations or dislocations. It can also show if the femoral trochlea has developed normally or if it is shallow.
MRI scan helps to assess the articular cartilage of the patella and knee joint. Any patellar malalignment or any injury to the patella-femoral ligaments is also seen on MRI scan.
CT scan may be done additionally to find out any possible cause for patellofemoral instability. 3D reconstruction allows to assess if any patella-femoral joint malalignment exists and also its severity.
Patients with patellofemoral instability have problems with the alignment of the patella. Therefore, treatment is necessary to bring the patella back into normal alignment. It can either be conservative or surgical based on clinical examination and investigation findings.
Conservative treatment:
It is indicated if there is patellar subluxation (partial dislocation).
- Painkiller medications are recommended to be taken as required
- Rest from stressful activities
- Ice or warm fomentation
- Physiotherapy- helps to strengthen the quadriceps muscles and improve the tracking of the patella. Various taping techniques are also used to improve or maintain patellar tracking.
- If the patella is completely dislocated, it needs closed reduction under anaesthesia to relocate it within the femoral trochlear groove.
- A specialised knee brace may be used to hold the patella reduced
Surgical treatment:
Surgery is sometimes needed to help return the patella to a normal tracking path when other non-surgical treatments have failed. The aim of the surgery is to realign the patella in the groove and to decrease the Q angle.
Dr Jadhav will decide which procedure is appropriate for a particular patient’s situation based on clinical examination and investigation findings.
Patellar realignment surgery is broadly classified into proximal re-alignment procedures and distal re-alignment procedures. These may need to be done in isolation or in combination.
Proximal re-alignment procedures:
During this procedure, structures that limit the movements on the outside of the patella are lengthened (lateral release) or ligaments on the inside of the patella are shortened (medial plication). In selected cases with femoral groove malformation and shallowness, femoral trochleoplasty gets done.
Distal re-alignment procedures:
In cases with severe knee malalignment, the Q angle is decreased by performing a procedure called a tibial tubercle transfer (TTT). In this procedure the tibial tubercle with its attached patellar tendon is removed and re-attached to the medial portion of the upper tibia using screws.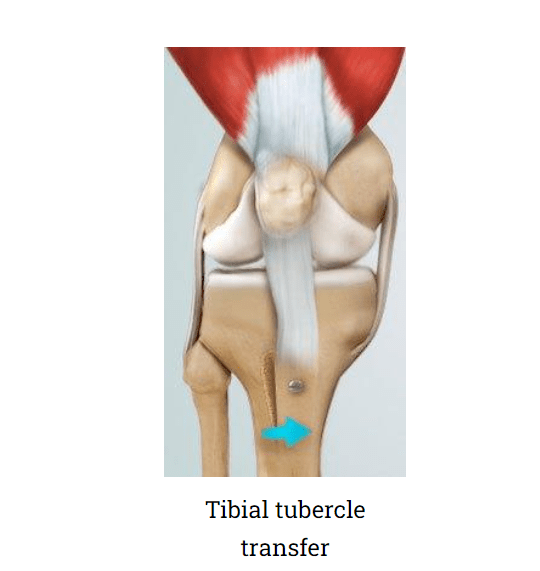
The realignment surgeries are performed under sterile conditions in the operating room under spinal or general anaesthesia. The surgeon will make two or three small cuts around your knee. The arthroscope, a narrow tube with a tiny camera on the end is inserted through one of the incisions to view the knee joint. Specialized instruments are inserted into the joint through other small incisions. The camera attached to the arthroscope displays the image of the joint on the monitor. A sterile solution will be pumped into your knee in order to stretch the knee and provide a clear view and room for the surgeon to work.
With the images from the arthroscope as a guide the surgeon can look for any pathology or anomaly and repair it through the other incisions with various instruments. After the evaluation is completed and depending on your situation, a lateral retinacular release may be performed. In this procedure, the tight ligaments on the outer side of the knee are released, thus allowing the patella to sit properly in the femoral groove.
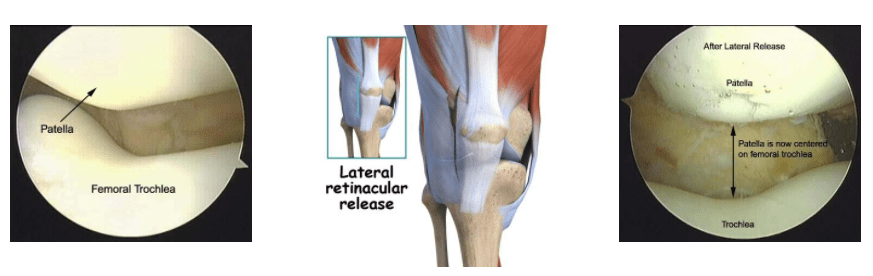
Lateral Patellar Lateral release & realignment of the patella
The surgeon may also tighten the tendons on the inside (medial side) of the knee (medial plication) to realign the quadriceps. Both these procedures can be done arthroscopically or through mini-open techniques. In severe mal-alignment of the knee, the tibial tubercle transfer gets done additionally.
The surgical steps should properly realign the patella and allows it to sit well within the femoral groove. Once the malalignment is repaired and re-confirmed with arthroscopic vision, the incisions are closed with sutures. Sterile dressings are applied to the wounds and a compression bandage is given. Patient’s knee is protected with a range of motion knee brace.
- Painkiller medications to given to relieve pain.
- Regular icepacks are applied 4 to 5 times a day
- The operated leg is kept elevated to reduce swelling and pain.
- Patients use their knee brace for support and mobilise non-weightbearing with a pair of elbow crutches for 4 to 6 weeks. They are taught exercises to be done when lying in bed and also when sitting in a chair.
- Patients are advised about do’s and don’t’s during their recovery period
- Regular physiotherapy is needed for knee strengthening, regaining full knee mobility and making the patellofemoral joint stable. It helps in faster recovery.
The possible risks and complications associated with the surgery include:
- Loss of ability to extend the knee
- Recurrent dislocations or subluxations
- Arthrofibrosis (thick fibrous material around the joint)
- Persistent pain
- Swelling
- Blood clot in legs
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

