Meniscus Injuries
& Management
Meniscus is a wedge shape piece of cartilage present in the knee joint between the femur (thighbone) and the tibia (shinbone). One meniscus is present on the inner side of the tibia and called the medial meniscus. It appears like the letter C when seen from the top. Its front and back ends are firmly attached to the top surface of the tibia. The entire outside or peripheral portion of the medial meniscus is attached to the knee joint capsule
The other meniscus, present on the outer side of the tibia, is the lateral meniscus. It is shaped like letter D. It is also attached to the top surface of the tibia as well as the capsule but is relatively more mobile than the medial meniscus.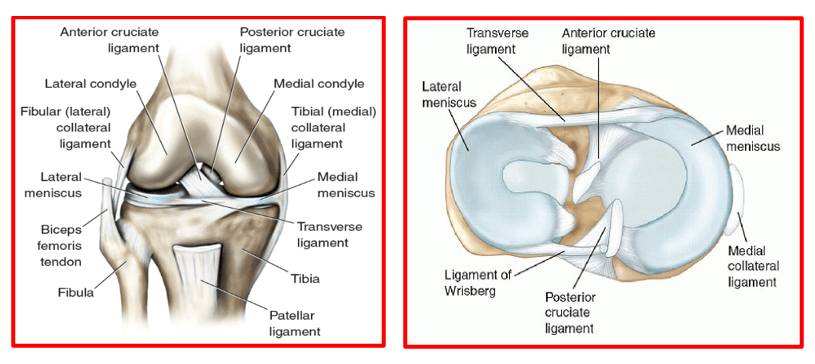
The menisci act as shock absorbers for the knee by spreading compression forces from the femur over a wider area on the tibia. They also help in stabilising the knee.
The medial meniscus bears up to 50% of the load applied to the medial compartment of the knee.
The lateral meniscus absorbs up to 80% of the load on the lateral compartment of the knee.
During the various phases of the walking cycle, forces shift from one meniscus to the other, and forces on the knee can increase to 2 – 4 times body weight.
While running, these forces on the knee increase up to 6 – 8 times body weight. There are even higher forces when landing from a jump.
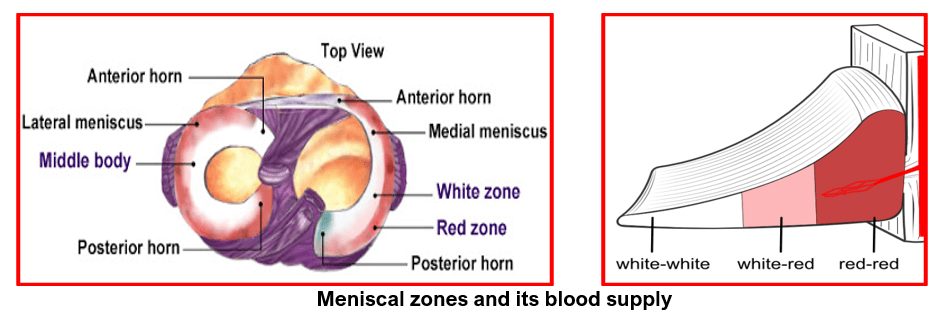
Each meniscus has 3 regions: anterior (front), posterior (back) and the middle region.
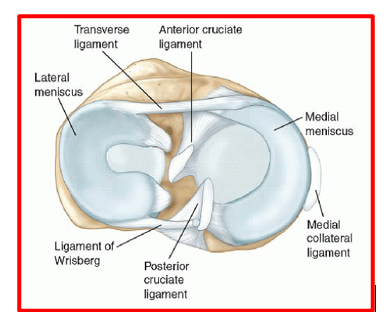
The anterior region has an anterior root, the anterior horn and anterior part of the body. Similarly the posterior region has a posterior root, the posterior horn, post part of the body. The middle region of the meniscus forms the body of the meniscus.
The roots attach the front and back ends of both menisci firmly to the top of the tibia on inner (medial) and the outer (lateral) sides.
The entire periphery of the medial meniscus is attached to the joint capsule and a portion of the inner ligament (deep medial collateral ligament). The lateral meniscus peripheral portion is also attached to the knee joint capsule except for a small area where the popliteus tendon separates it from the capsule. This peripheral attachment difference makes the lateral meniscus relatively more mobile compared to the medial meniscus.
The menisci derive their blood supply from the peripheral blood vessels. These vessels travel inwards from the periphery to the central free portion. This peculiar pattern of blood supply creates 3 zones of variable blood supply within the meniscus.
- The outer or peripheral zone of the meniscus has maximum blood supply and hence called ‘red on red’
- The middle third zone has lesser blood vessels compared to the peripheral portion. This mixed zone is called ‘red on white’
- The inner free edge of the menicus has no blood supply. Hence it is called the ‘white on white’ zone
Meniscus tear is the commonest knee injury in athletes and at any age in active people, especially those involved in contact sports. A sudden bend or twist in your knee cause the meniscus to tear. This is a traumatic meniscus tear. Such tears can occur either in the medial meniscus or the lateral meniscus or in both menisci.
Elderly people are more prone to degenerative meniscal tears as the meniscus weakens with age. Such tears are usually seen in the posterior horn of the medial meniscus and are often complex tears.
A torn meniscus can cause pain, swelling, stiffness with catching or locking sensation in the knee. Patients are unable to move their knee through its complete range of motion. Patients may have a limp or difficulty in walking. Meniscal tears may occur in isolation after an injury or they can occur along with other knee injuries like ligament injuries, cartilage injuries or fractures around knee.
Meniscal tears are diagnosed on careful medical history, clinical examination, X-rays and a knee MRI scan. Sometimes they are seen during knee arthroscopy.
X-rays may be normal in the acute cases or show presence of any fractures. They may show signs of calcium deposits in the meniscus in cases of pseudo-gout (chondrocalcinosis).
MRI scan helps to confirm the meniscal tear & its type, shows any other co-existing injuries and also the presence of any peri-meniscal cysts.
Meniscus tears, as seen on knee MRI, are classified into three grades. Grades I and II are not considered serious. They may not even be apparent with an arthroscopic examination. Grade III is a true meniscus tear and an arthroscope is close to 100 percent accurate in diagnosing this tear.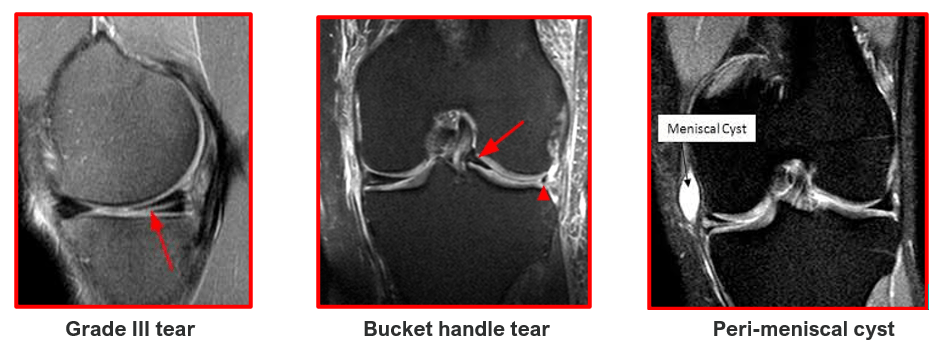
The various types of meniscal tears are: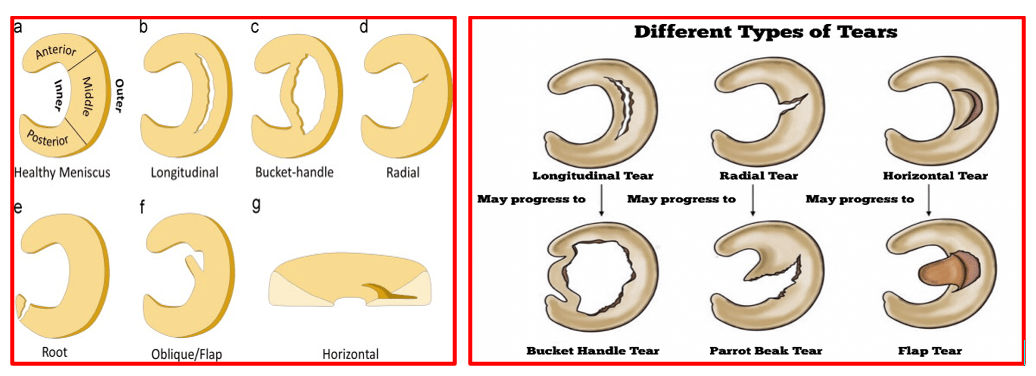
The types of meniscal tears depend upon their appearance and also the locations of the tears.
These tears are described as longitudinal tears, bucket handle tears (when the torn portion flips inside the joint), radial tears, parrot beak tears, horizontal tears, oblique or flap tears, root tears and complex tears (which is caused by combination of other tear patterns).
Degenerative tears are also a type of tear where the torn meniscus is ragged and tend to occur in older people with pre-existing degeneration of the cartilage.
The treatments for meniscal tears can be non-surgical or surgical.
These treatments depend on the type, size and location of tear as well the patient’s age and activity levels.
The patients are initially given suitable painkiller & anti-inflammatory medications to reduce their pain and swelling in the acute scenario. They are advised to rest the knee and do regular ice-packing throughout the day. Patients are taught physiotherapy exercises and allowed knee movements as tolerated. They may or may not need crutches for walking.
Patients who have small tears, peripheral tears, tears classified as Grade I or II (on the MRI) and degenerative meniscal tears in the elderly are given this non-surgical treatment. Their pain and knee swelling gradually settle down over 4 to 6 weeks. They can be back to their usual activities by 2 to 3 months.
Patients with Grade III meniscal tear patterns on the MRI, displaced bucket handle tears, tears of the anterior or posterior roots of the meniscus, tears associated with discoid menisci, grade III meniscal tears associated with other ligament or cartilage injuries and meniscal tears associated with fractures are advised surgery.
Patients, who are treated initially with conservative methods and whose symptoms do not resolve with non-surgical treatment, may also be advised surgical treatment e.g. the degenerative posterior horn tears in the elderly.
What types of surgeries are done for meniscal injuries?
The surgical treatment options for meniscal injuries include
- Partial Meniscectomy:
Injured part of meniscus, that is of poor quality & is irreparable, gets removed. The healthy peripheral part is left behind.
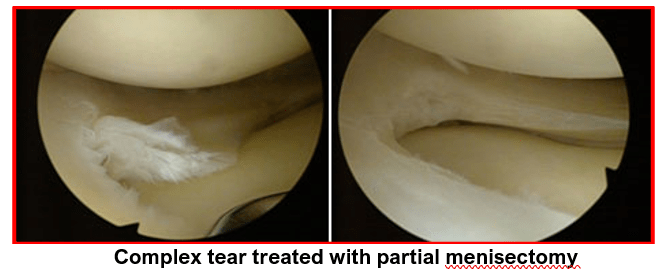
Complex tears, degenerative tears, radial tears and discoid meniscus with central degenerative tear patterns are not amenable to repair and need partial menisectomy.
Failed meniscal repair on 2 occasions also warrants partial menisectomy.
Long-term consequences of menisectomy:
If the menisci are removed, the forces are no longer distributed over a wide area of the tibia.
Without the medial meniscus, the tibial contact area is decreased 50 – 70%. This means the same forces from the femur are concentrated on a smaller area of the tibia.
When the lateral meniscus is removed, there is a 45 – 50% decrease in contact area. This results in a 200 – 300% increase in contact pressure, which can eventually damage the cartilage on the ends of the bones. This can lead to degenerative arthritis.
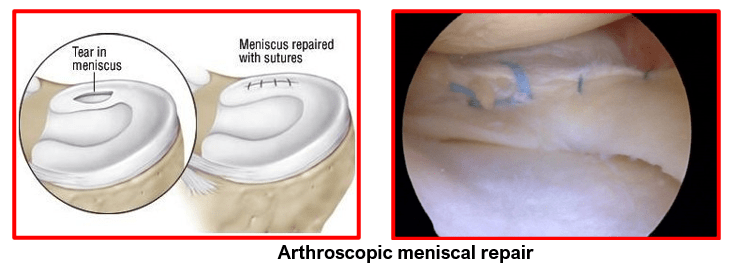
2) Meniscus Repair:
The torn meniscus tissue is repaired with special non-absorbable sutures using specialised instruments and different repair techniques.
Used in these circumstances:
- Peripheral tear in the red on red zone
- Vertical and longitudinal tears
- Bucket handle meniscus tear
- Tears that are 1-4 mm in length root tear
- Acute repair combined with ACL reconstruction
- Tears associated with tibial plateau fractures
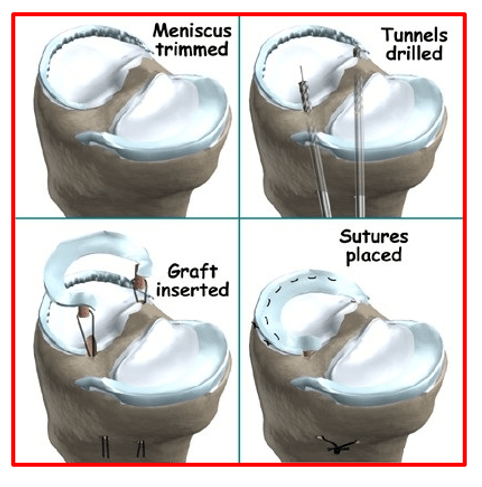
3) Meniscus Replacement / Transplantation:
Complete meniscal tissue with bony plugs, harvested from cadavers, gets inserted and secured inside the knee in the affected compartment. Used in young patients, with previous partial menisectomy, without significant arthritic changes.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

