Knee Arthritis and Total Knee Replacement
Knee Arthritis is a condition wherein the smooth articular cartilage, that covers the lower femur and the upper tibia, is worn out exposing the underlying bones. This causes the bones to rub against each other and leads to pain, swelling and deformities of the knee joint.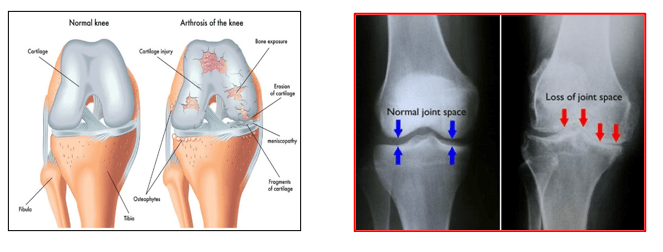
The common causes of knee arthritis are:
- Osteoarthritis – this is age related wear and tear of the knee joint. Commonly affects people older than 50 years of age and may run in families.
- Rheumatoid arthritis – this is an auto-immune disorder that attacks the articular cartilage of the knee joint. There is inflammation and thickening of the synovial membrane. This inflamed synovial membrane produces excess synovial fluid which overfills the joint. Chronic inflammation, pain and stiffness arise as the joint cartilage gets damaged further.
- Post Traumatic arthritis – results due to fractures and injuries around the knee joint that affect the joint surfaces of the articulating bones e.g. Tibia, Femur or patella. Instability in the knee due to ligament injuries can also lead to damage to the articular cartilage. Additionally, damage to the cushioning discs within the knee joint (meniscus) can also lead to joint arthritis in the long term.
Patients with knee arthritis will have:
- Deep aching chronic joint pain during movements and later also at rest.
- Swelling and warmth around the joint
- Stiffness in the joint, especially in the morning
- Difficulty in walking, sitting or squatting on the floor, crossings their legs or using the stairs. They may have difficulty in using Indian toilets
- Patients have disturbed sleep due to pain
- They also notice deformities of their knees and have limp whilst walking
- They may have feeling of locking/catching or giving way.
- Crunching or grinding during their knee movements
The diagnosis of knee arthritis is based on detailed medical history of the patients, their symptoms, typical findings on clinical examination of knee and x-rays of their knee.
CT and MRI scans have limited role in the diagnosis of knee arthritis. But MRI scans can help identify degenerative or post-traumatic tears in a patient with knee arthritis. It can also pickup certain pathologies of the synovial membrane that may be causing the knee arthritis.
The non-surgical (conservative) treatments for knee arthritis are as follows:
- Activity modifications – patients are educated about their disease and taught lifestyle modifications to reduce their pain and keep it under control. Pain inducing activities like squatting, kneeling, sitting cross legged, sitting on the floor and repeated use of stair are avoided. Patients are encouraged to use a commode instead of an Indian style toilet. Patients can learn to lead an active lifestyle with some minor changes to their routine activities.
- Walking aids – use of a walking stick or a single crutch helps offload stress on the arthritic knee joint. Generally, stick is used on the same side of the painful knee. Patients get a sense of stability, have reduced knee pain and are able to mobilise better.
- Physiotherapy – helps in strengthening the muscles around the knee joint. This helps in reducing pain, improving knee range of motion and improved patient mobility. Regular exercise does not worsen the arthritis. If patients doing regular knee exercises go on to have knee surgery in later stages, they recover faster.
- Anti-inflammatory and Pain-killer medications – these help in controlling pain and reducing inflammation. This results in improved mobility. There are various types of medications available for pain control. These medications are prescribed taking into account the patient’s pain intensity, health profile and his safety. All such medications must be taken as per doctor’s advice and instructions.
- Weight reduction – Very important step but difficult to follow. Reducing weight reduces the load on the knee, reduces pain and improves knee mobility. Roughly 1 kg loss of weight means 3 kgs less load on the knee joint. Obesity brings its own set of problems when patient comes for knee replacement surgery.
- Chondro-protective agents – Glucosamine and chondroitin sulphate are considered as chondro-protective medications. These slow down the process of arthritis and thought to help in regrowth of the cartilage. This helps in pain relief. These medications need to be taken together in appropriate doses for best possible result.
- Visco-supplementation – This involves injecting the knee joint with special liquids (hyaluronic acid) that increase the viscosity of the joint fluid and improve the health of the knee cartilage. This leads to improved joint lubrication and reduced friction between the arthritic surfaces of the knee joint. Minor cartilage lesions are thought to heal with such injections. Their pain-relieving effect lasts for 6 months to 12 months. Ideally most useful for early stages (mild to moderate) knee arthritis in young patients. Based on their viscosity these injections can be a single dose or multiple dose therapy.
- Cortico-steroid injections – help in reducing pain, inflammation and swelling in arthritic knees, especially to rheumatoid arthritis or osteo-arthritis. Multiple injections must be avoided for the risk of infection in the knee joint.
Knee replacement is indicated when there is:
- Moderate to severe arthritis with knee pain that is limiting patient’s normal activities of daily living e.g. walking, using stairs, getting in and out of chairs.
- No improvement in pain even after taking regular pain killers, using walking aids, reducing activities or changes in lifestyle
- Harmful side-effects from pain-killer medications
- No improvement in pain with physiotherapy, weight loss, visco-supplementation or steroid injections
- Severe pain that causes restriction of social life with sense of being house bound and dependent on others to lead a normal life.
- Confirmation of advanced arthritis on x-rays in a symptomatic patient
Knee Replacement surgery benefits patients in many ways.
This surgery helps to:
- alleviate or remove knee pain
- improve patient mobility and functions
- correct pre-operative angular deformities of the knee
- improve quality of life and return patient to normal daily activities
- make patients independently mobile and self-reliant. They do not have to depend on family members or nursing care for their activities of daily living.
Yes, both knees can be replaced at the same time. The patient should be medically fit, relatively younger and having knees without severe or complex knee deformities.
Bilateral knee replacement offers few advantages to the patient:
- Saves cost
- Avoids need for separate second hospitalisation
- Post-surgery rehabilitation time is same as that in a single knee replacement
- Overall return to normal life is faster.
Getting informed: Find out about your standard of room in the hospital where your surgery is planned. Confirm if a relative can stay with you at all times or only within restricted hours. Get to know what type of anaesthesia will be used for your surgery. Try to know more information about your type of surgery. Sometimes it may be helpful to speak to or to meet a patient who has undergone a similar operation from your surgeon.
Arrange for home help. Seek help from a relative or a nurse/attendant (who are trained and experienced) for few weeks to help you at home after our discharge from the hospital.
Arrange for transport: Arrange for someone to take you to and from the hospital in a comfortable vehicle.
Prepare your home: Prepare your bed and chair where you would be spending most of your time, after surgery. Have appropriate walking aid ready when for you return home. Get your commode fixed with a seat raiser and any side supports if needed. If you have an Indian type toilet then get a temporary foldable commode seat fixed to the wall or use a commode chair. If possible, arrange everything on a single floor, preferably ground floor, until you become fully mobile again.
Clean up: Before going to the hospital, have a good bath or shower, cut and clean your nails, and put on freshly washed clothes. These measures help prevent unwanted bacteria from going with you to the hospital and complicating your care.
The actual surgical procedure takes about 45 to 60 minutes for a single side knee replacement.
Pre-operative precautions, preparations, surgical and recovery time in recovery room may take 2 to 3 hours in total.
There are 3 types of anaesthesia that may be used for performing a total knee replacement. These are General, Spinal or Epidural anaesthesia.
The type of anaesthesia used for you will be decided by the anaesthetist after checking your physical status and investigations for surgical fitness. Final choice is decided after consultation with you.
Generally, knee replacement surgeries are done under epidural anaesthesia or a long acting spinal anaesthesia with post-surgery nerve blocks. The area below the waist is made numb for the operation. After getting and epidural anaesthesia, the patient may decide to stay awake fully or have a sedative injection. Epidural anaesthesia is continued via a special catheter tube and a special syringe pump for next 2 to 3 days. This allows good pain relief. Knee exercises can be started in bed without pain. This helps patient’s confidence about physiotherapy and improves their cooperation and performance.
- Total knee replacement surgery is performed in a suitably informed, consented and anaesthetised patient.
- All sterile preparations are done in a standardised manner using disposable drapes and gowns.
- A midline skin incision over the front of the knee is made and the joint is exposed.
- The surgeon removes the damaged bone and cartilage from the femur and the tibia. Precision cutting blocks and jigs, as per each patient’s size, are used for cutting and preparation of the bones. If necessary, the inside of the patella is also shaved off and prepared to take a plastic implant.

- The knee joint is then reconstructed using artificial implants to give correct alignment, knee stability and good range of knee motion. These implants are fixed to their respective bones using a special glue called bone cement (polymethylmethacrylate). This artificial joint now starts functioning like a normal joint.
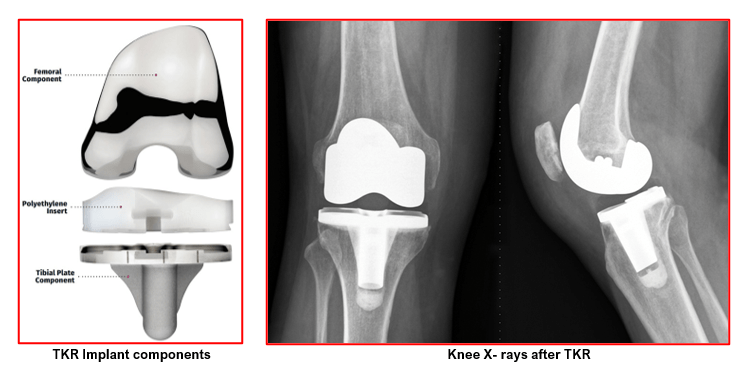
In a typical knee replacement:
- The femoral implant is made of highly polished cobalt chrome
- The tibial implant (baseplate) is made up of titanium or cobalt chrome.
- High grade plastic (polyethylene) insert is locked onto the tibial baseplate
- Patella is resurfaced using a high-grade plastic button.
- The knee wound is closed in layers and a sterile dressing is applied. Compression bandage is given over the top and patient is shifted to recovery room for observations.
Newer designs and implants keep coming into the market enabling higher flexion (knee bending), better function and implant longevity.
Dr Anand Jadhav will select the best implant for you after proper consultation and counselling.
The physiotherapist will help you to get up and walk about as quickly as possible. Next day after your surgery, you may be able to sit on the edge of the bed, stand and even walk with help. You have to use a walker initially and then move onto crutches if your progress is satisfactory. You will be taught to walk to and from the toilet and also in using the commode. A seat raiser for the commode is needed for 2 to 3 months. You will be taught to use stairs as well with help of crutches.
It is normal to experience discomfort while walking and exercising. Your legs and feet may be swollen. A physiotherapist will teach you exercises to help strengthen the knee and explain precautions to be taken.
Most patients will need to use crutches or a walker for about 4 to 6 weeks or until instructed otherwise by their physiotherapist.
The joint pain that you had before the surgery will go away immediately, but there will be a different type of pain due to the operation. This post-operative pain will be temporary and is well controlled with pain-killer medications either in the form of injections or tablets.
Your hospital stay will be around 3 to 4 days for a single side knee replacement surgery. For bilateral knee replacement surgeries (done in a single stage) your stay will be between 5 to 7 days, depending on your fitness and progress following the operation.
A complete discharge summary along with written instructions for medications, follow-up visits and physiotherapy guidelines will be given to you on discharge.
To ensure a comfortable and trouble-free recovery, we recommend a list of modifications at your home prior to discharge:
- Handrail in your bathroom. Bathroom must be kept dry and non-slippery. A stable chair for shower.
- Stairways must have handrails
- A stable chair with a firm seat cushion, a firm back, two arms, and a footstool for intermittent leg elevation
- A commode seat riser with arms should be fitted.
- If you have an Indian toilet, a commode chair or a foldable toilet seat needs to be arranged.
- All loose carpets and cords must be removed from home
- Living, bedroom and bathroom to be on the same floor preferably, because walking up or down the stairs will be difficult during early recovery
Your physiotherapist will instruct you about simple home exercises and also the frequency of doing these. These exercises help in developing strength of thigh muscles and increasing range of knee joint movement. Regular walks are also necessary. The knee should have icepacks for 20 minutes 4 to 5 times a day. The joint should be kept elevated while at rest. Patients should follow these instructions to avoid over-exercises which can cause more pain or swelling.
Your wound gets inspected and the dressing changed, prior to your discharge. This new dressing can be left undisturbed till the time of suture removal. Sutures or skin staples are removed 14 days after surgery.
You can have a bath or shower generally 2 weeks after the operation when wounds have been checked for healing and all sutures or skin staples have been removed. Until then we advise sponging without getting the operative wound wet.
You should be able to get rid of the crutches by 4 to 6 weeks and feel more or less normal by three months. Normal daily activities of living become easier. Always take advice from your surgeon and physiotherapist before beginning any new activity.
It depends on your progress, but usually after about 4-6 weeks. You need to have pain-free knee joint, sufficient muscle strength and good knee joint motion prior to driving. Please consult Dr Jadhav for further advice.
It depends on the type of your job and recovery from surgery. Most office-type workers can resume work in 4-6 weeks.
Usually 6 weeks after your knee replacement, you need to meet Dr Jadhav for a check-up. He will examine your operation site, your walking, your balance and muscle strength.
Dr Jadhav will then see you at 3 months, 6 months and 1 year following your surgery. X-rays will be done during these visits to check that all is well.
Subsequent follow-ups are advised after 5 and 10 years with new x-rays of your knee replacement to see for any signs of loosening.
- After a total knee replacement, patients experience a remarkable reduction of knee pain. There is improvement in the ability to perform activities of daily living without the need of help from others. They feel confident and have an improved social life.
- You can bend the operated knee upto 90-100 degrees easily within first 2 to 3 weeks. This amount of knee bending can allow you to get in and out of a chair or use stairs. The amount of knee bend after surgery depends upon how much mobility you had prior to your surgery. Certain modern implants can give you additional bend, but you will not get full knee bending as in a normal knee.It is common for some patients to have a sense of stiffness for initial few weeks after knee replacement.
- Some swelling can persist on the operated leg for 6-9 months.
- A small area of numbness around knee is also common but this sensation does not bother patients.
- It can take 2- 3 months before you feel near normal again. You should be prepared to continue home exercise for 4-6 months.
- You need to understand that total knee replacement will not allow you to do more than what you were able to do before you developed arthritis. You must avoid certain activities like jogging and high-impact sports for the rest of your life.
- With normal use and activity, every knee replacement develops some wear in its plastic cushion. Excessive activities or increased body weight may accelerate this normal wear. This may cause the knee replacement to loosen and become painful.
- With appropriate activity modifications, modern knee replacements can last minimum up to 15 to 20 years.
After knee replacement surgery you should contact Dr Jadhav if you notice any fever or chills ( 38° C or 100.4° F), persistent warmth or redness around the knee, discharge (leakage) from wound, persistent or increased pain in the knee or calf muscle pain and shortness of breath.
Possible risks during Knee Replacement surgery are:
Risks for any anaesthesia are:
Allergic reactions to medicines
Breathing problems
Risks for any surgery are:
Blood clots in the legs (DVT- deep vein thrombosis) that may travel to the lungs (PE- pulmonary embolism)
Infection, including in the lungs, urinary tract, and chest
Bleeding
Some risks of this surgery are:
Infection of the knee joint
Wear of the artificial joint
Loosening of the artificial joint over time
Knee stiffness
Allergic reaction to the artificial joint
Injury to nerves - Some area of numbness develop over the outer aspect of knee. This numbness reduces in 4-6 months with return of normal sensations. Often a very small patch of numbness (the size on thumb nail) remains but this does not bother patients.
Injury to blood vessels
People who have a prosthesis, such as an artificial joint, need to carefully protect themselves against infection. You should carry a medical identification card in your wallet that says you have a prosthesis. You may need to take antibiotics before any dental work or invasive medical procedures.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

