Hip Avn – Avascular
Necrosis
of the Femoral Head
Avascular necrosis of the hip joint is a condition where there is reduction in the blood supply to the femoral head (ball part of the hip joint). As the blood supply gets cut off for any reason, the bone in the femoral head dies. Gradually it collapses under constant body weight and leads to deformity of the femoral head. Eventually the hip joint becomes arthritic and painful. Hip AVN generally affects people in the age group of 20-50 years.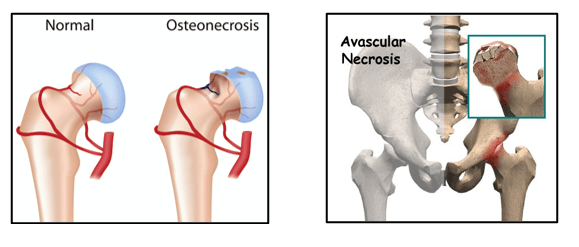
Hip AVN can arise due to traumatic and non-traumatic reasons.
Post-traumatic AVN:
Fractures of the neck of the femur – in such cases the blood vessels supplying blood to the femoral head are damaged or cut off. This leads to bone necrosis, subchondral fractures and collapse of the femoral head.
Hip dislocations – the capsular blood vessels get damaged leading to AVN in about 20 % of patients.
Non-traumatic AVN: Here the smaller blood vessels supplying blood to the femoral head get clogged due to tiny fat globules. This blocks the supply of blood and oxygen to the femoral head, which dies and collapses. (This situation is similar to blockage of a water supply pipe with tiny sand particles stopping the flow of water).
Common risk factors for AVN are:
- Alcohol abuse
- Corticosteroids
- Gaucher’s Disease
- Diabetes
- HIV/AIDS
- Sickle Cell Disease
- Pancreatitis
- Chemotherapy/radiation therapy
- Autoimmune deficiencies/diseases
- Hypertension
- Vasculitis
- Caisson Disease
- Patients may be asymptomatic in the early stages.
- Patient may complain of hip region pain which could be localised to the lower back, groin or the outer upper side of the hip and thigh region. This pain may occur on exertion or walking. In later stages it can be present constantly.
- The local of pain can mislead a surgeon to think that the pain is coming from the spine rather than the hip joint. Pain may disturb patient’s sleep and also affect his quality of life.
- There will be limp and difficulty in walking far or sitting in one position for a long time.
- As the femoral head collapse there will be shortening of the affected leg and postural scoliosis (sideways curvature of the back).
- The hip movements are painful the range is also reduced as the AVN advances.
- There will be limb leg inequality due to shortening of affected side.
- Surgeon needs to thoroughly examine both hips, knees and spine of the patient to be sure that the source of the patient’s problem is indeed the hip joint.
Diagnosis of Hip AVN is made on the basis of detailed medical history, thorough clinical examination of the patient, appropriate blood tests, X-rays of both the hips joints and MRI scan of the hip joint.
Spine x-rays may also be needed to rule out spine problems as the source of the pain.
X-rays of the hip joint will be normal in the early stages of AVN. Changes may take 6 to 9 months to be apparent on the x-rays.
MRI helps in diagnosing hip AVN at a very early stage. It is useful for staging the disease process and also for guiding appropriate management.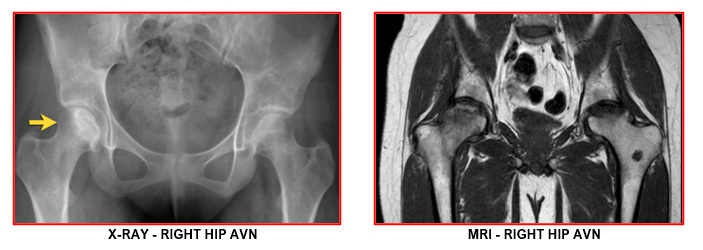
Occasionally Bone scan or CT scan of the hip may be needed in Hip AVN patients.
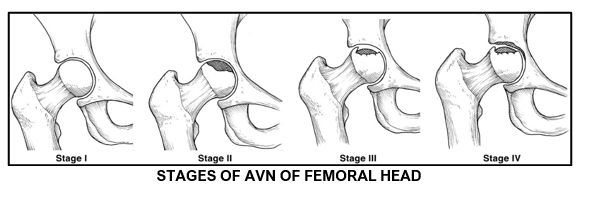
We can diagnose avascular necrosis and stage it with x-rays and MRI of the hip joints. There are four stages indicate the level of the disease and if it has progressed. Treatment plans gets individualised based on these stages.
Stage I Normal x-rays but MRI reveals the dead bone.
No collapse of femoral head
Stage II Can be seen on regular x-ray and MRI.
No collapse of the femoral head.
Stage III Signs of collapse (called a crescent sign) seen on x-ray.
Stage IV Femoral head collapse on x-ray and signs of cartilage damage
(osteoarthritis).
The non-surgical treatments of hip AVN are used initially for all stages:
- Painkiller and anti-inflammatory medications are given for few days to weeks to control pain and improve mobility.
- Activity modifications
- Walking stick or elbow crutches are recommended as necessary.
- Physiotherapy as tolerated
- Anti-osteoporosis medications are taken to prevent /delay bone collapse
The surgical options for management of hip AVN are core decompression surgery and hip replacement surgeries. These patients should have had failure of conservative treatment before being taken up for any surgery.
Core decompression surgery – Recommended for symptomatic Stage I and II AVN patients without any signs of femoral head collapse.
A suitably selected and consented patient is taken for surgery on a specialised fracture table which allows use of an image intensifier (c-arm machine).
With small incision, the outer part of upper femur is exposed. Under x-ray control small diameter drill wires are inserted into the femoral head areas with AVN changes. After confirming satisfactory position of the wire, a drill is inserted over the guide wire and drilled until just short of the joint surface without breaching it. Multiple such drilling is done in 3 to 4 areas of the necrotic area.
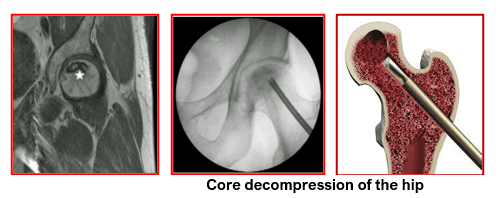
Mere drilling of the bone creates a decompression effect by relieving the built-up pressure within the confines of the rigid bony boundaries of the upper femur. This sudden reduction in pressure gives dramatic pain relief which is the immediate positive effect of the core decompression surgery.
Additionally, there is removal of dead bone along the drill track areas. This opens up new channels for regrowth of new blood vessels into these tracks. These vessels bring fresh blood supply and repair materials into the necrotic bone areas of the femoral head. This leads to formation of bony bridges along the drill tracks. These new bony bridges behave like bamboo sticks supporting a roof-top and preventing it from collapsing. Core decompression thus delays the collapse of femoral head and also gives good pain relief. The need for a hip replacement surgery is also delayed.
Newer techniques have been developed to encourage and ensure bone re-vascularisation, building of new bony bridges in the areas of bone necrosis and prevention of femoral head collapse. These involve filling up of the drill tracks with any of the below techniques:
- Platelet Rich Plasma (PRP) - This is produced from patient’s own blood, using a specialised machine within the OT. This is an effective and cheaper addition to plain core decompression. Enhances new bone formation. Works for 5 to 7 years depending upon stage of AVN and timing of surgery
- Bone Marrow Aspirate (BMAC) - Patient’s own bone marrow cells are aspirated from the pelvis bone and concentrated in a machine before injecting into the drill tracts just like the PRP. Has similar results to that of the PRP injections.
- Cultured (cultivated) Osteoblasts – This is a two staged procedure.
Stage 1: is done as a day care procedure 4 weeks prior to core decompression. Patient’s own bone marrow cells are harvested from the pelvis bone and sent to a specialised lab for cultivation (multiplication) of bone forming cells, called osteoblasts.
Stage 2: These cultured osteoblast cells are injected into the drill tracts at the time of core decompression surgery. Generally, for these cases, a single large size drill is used within the centre of the AVN area. After clearing the drill tract of dead tissue, the osteoblasts are injected into the predrilled tract and the outer drill hole is sealed to trap the osteoblasts within the bone.
New bone forms in this drill tract and supports the femoral head cartilage. This new bone helps prevent collapse of the femoral head. Though expensive, this technique has shown encouraging results lasting from 10 to 15 years post-surgery. It thus delays the need for total hip replacement for many years, especially in the younger patients.
Dr Jadhav prefers to perform either of the above procedures after routine core decompression surgery. The choice of these additional measures depends upon patient’s counselling, wish and affordability.
HIP REPLACEMENT SURGERY:
Total Hip Replacement (THR) – This surgery is recommended for:
- patients who have advanced arthritic changes at first presentation
- patients who have failed to respond to conservative management and are getting worse symptomatically
- patients who have worsened after a successful core decompression surgery in the past and now having advanced arthritis
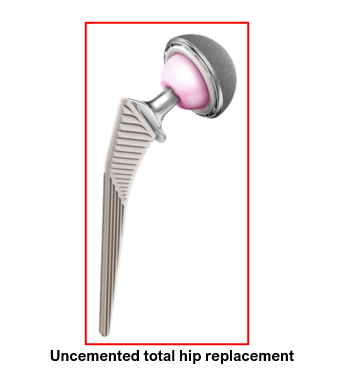
This is the last resort but gives best pain relief, increased mobility and improved hip range of motion. It allows patients to live an active and independent lifestyle.
As many of these patients are young, most of them require uncemented total hip replacements which can function for as long as 20 to 25 years.
The benefits of PSI technology for Total Knee Replacement are significant in terms of optimised patient outcomes, safety and healthcare economics.
- Use of advanced software that allows 3D reconstruction of the joint and supports all
implant sizes
- The restoration of the mechanical axis
- Special consideration given to the rotational alignment of the tibial tray
- Optimised patella tracking
- Personalised posterior slope
- Restoration of the joint kinematics
- Disposable instrumentation
- Minimised risk of cross contamination
- Instrument sterilisation & processing costs are saved
- Replacement / refurbished instrumentation not needed saving costs
The benefits of PSI technology for Total Knee Replacement are significant in terms of optimised patient outcomes, safety and healthcare economics.
- Use of advanced software that allows 3D reconstruction of the joint and supports all
implant sizes
- The restoration of the mechanical axis
- Special consideration given to the rotational alignment of the tibial tray
- Optimised patella tracking
- Personalised posterior slope
- Restoration of the joint kinematics
- Disposable instrumentation
- Minimised risk of cross contamination
- Instrument sterilisation & processing costs are saved
- Replacement / refurbished instrumentation not needed saving costs
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :