Chondromalacia Patellae
Chondromalacia patellae is a condition where there is abnormal softening of the cartilage on the under-surface of the patella (kneecap). It is one of the most common cause of chronic knee pain. This condition is common among young, athletic individuals, but may also occur in older adults who have arthritis of the knee.
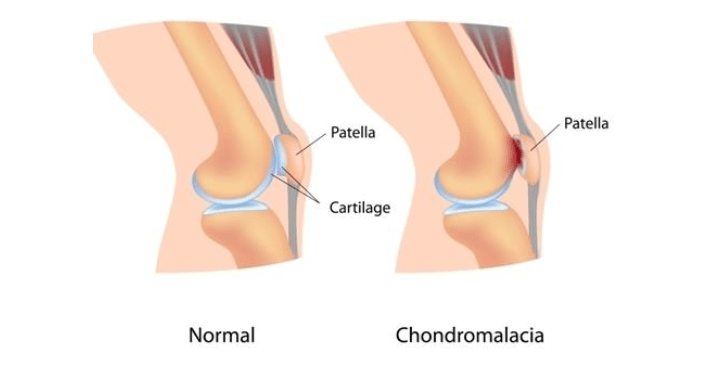
Your patella normally resides over the front of the knee joint. When the knee joint is bent your knee, the backside of your patella glides over the cartilage of the lower femur (thigh bone). Tendons and ligaments attach the patella to the tibia (shinbone) and quadriceps (thigh muscle). When any of these components fails to move properly, it can cause the patella to rub up against the femur. This abnormal rubbing can lead to deterioration of the patellar cartilage, resulting in chondromalacia patellae.
Improper patellar movement may result from:
- poor alignment due to a congenital condition
- weak quadriceps (muscles at front of thigh) and hamstrings (muscles at back of thigh)
- muscle imbalance between the adductors (muscles on the inside of the thigh) and abductors (muscles on the outside of the thigh)
- repeated stress on the knee joint due to running, skiing, or jumping,
- a direct blow or trauma to the patella
Factors that may increase the risk of developing chondromalacia patellae:
Age
Adolescents and young adults are at high risk for this condition. During growth spurts, the muscles and bones develop rapidly, which may contribute to short-term muscle imbalances.
Sex
Females are more likely than males to develop chondromalacia patellae, as they typically possess less muscle mass than males. This can cause abnormal knee positioning, as well as more lateral (side) pressure on the patella
Flat feet
Having flat feet may place more stress on the knee joints than having higher arches would.
Generalised Hyperlaxity of joints
Allows excessive sideways mobility of the patella. This increases the stress on its articular cartilage and leads to chondromalacia
Previous injury
A prior injury to the patella, such as a dislocation, can increase the risk of developing chondromalacia.
High activity level
High activity levels or engagement in frequent exercises place high pressure on the knee joint and the patella increasing the risk for chondromalacia
Arthritis
Chondro-malacia can also be a symptom of arthritis, a condition causing degeneration of the patellar cartilage and inflammation of the knee joint. Inflammation can prevent the patella from functioning properly.
Patients with chondromalacia patellae will typically present with pain in the front of the knee region. Pain may worsen after sitting for a prolonged period of time or during activities that apply extreme pressure to the knees, such as standing for long periods of time, using stairs, squatting, sitting on floor or cross-legged or exercising. Patients may feel sensations of grinding or cracking when bending or extending their knees. Some may even develop swelling of the knee joint.
Chondromalacia patellae is commonly diagnosed based on patient’s history and clinical examination of the knee. The doctors look for leg alignment and position of knee and the patella in standing and lying down position. Resistive pressure on the under-surface of the kneecap is painful. They may even notice knee swelling and wasting (thinning) of the quadriceps muscles. Patients may have difficulty and pain when trying to fully extend their knees.
Investigations may be ordered to confirm and stage the severity of chondromalacia patellae.
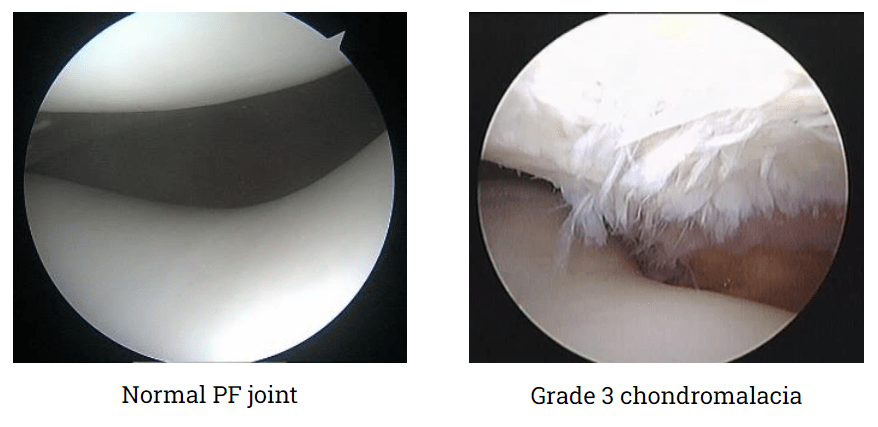
X-rays help in confirming mal-alignment or arthritis of the knee joint. Rarely an MRI becomes necessary. It shows the status of the articular cartilage of the knee and patella. Chondromalacia patellae can also get diagnosed during knee arthroscopy. The patellar cartilage shows signs of softening or various grades of wear and tear. Tilting and abnormal rubbing of the patella against the lower femur during movements of the knee joint can also be confirmed and documented during arthroscopy.
Grading of chondromalacia:
There are four grades, ranging from grade 1 to 4, that designate the severity of chondro-malacia. Grade 1 is least severe, while grade 4 indicates the greatest severity.
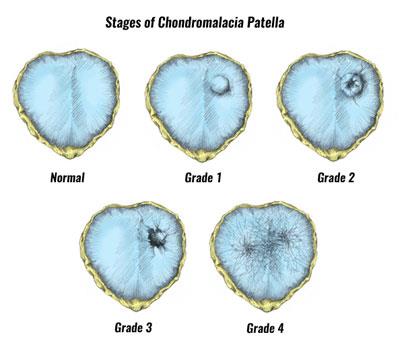
Grade 1- Indicates softening of the cartilage in the knee area.
Grade 2- Indicates a softening of the cartilage along with abnormal surface characteristics.
This usually marks the beginning of tissue erosion.
Grade 3- Shows thinning of cartilage with active deterioration of the tissue.
Grade 4- Indicates exposure of the bone with a significant portion of cartilage deterioration.
Bone exposure means bone-to-bone rubbing is likely occurring in the knee.
The goal of treatment for chondromalacia patellae is to improve the patellar tracking, reduce the pressure on the patella and the patella-femoral joint and reduce knee inflammation. This will lead to pain reduction, improved knee mobility and better function.
Conservative Treatments:
Rest & Lifestyle Modifications – pain producing activities are avoided and the knee gets rested. This can allow the cartilage damage to repair itself in early stages.
Patients are instructed to avoid squatting, kneeling, sitting on the floor or cross-legged, prolonged sitting, prolonged standing and repeated use of stairs.
Anti-inflammatory painkillers medications are prescribed as needed. This helps in reducing knee inflammation and pain. Allows patients to carry on their knee exercises without pain
Warm fomentation followed by light massage using analgesic gels are done twice a day. This helps ease the knee pain.
Physiotherapy is recommended even whilst the knee is painful. This helps in strengthening the inner portion of the quadriceps, hamstrings, hip adductors and abductors. With improved muscle strength and knee balance, there is improved patellar tracking and knee alignment. This leads to pain reduction.
Patients are also recommended non-weight-bearing exercises, such as swimming or riding a stationary bike. They are encouraged to do isometric exercises in bed. This involves tightening and releasing their knee and hip muscles which can help in maintaining muscle mass.
Surgical Treatments:
Arthroscopic knee surgery may be necessary to examine the joint and determine whether there is malalignment of the knee. This surgery involves inserting a camera into the knee joint through a tiny incision.
The patellar cartilage is examined, and the patellar tracking is noted. Any loose cartilage flaps can be trimmed, and the remaining cartilage edges are smoothened. A procedure called lateral release may be done if there is abnormal contact of the patella with the femur on the outside to the patella-femoral joint. This surgery reduces the lateral pressure and allows the patella to sit more centrally and track better over the lower femur. This reduces pain and improves knee strength.
Other surgical options for younger patients may involve implanting a cartilage graft to cover some deep patellar defects (cartilage transplant) or relocating the insertion of the thigh muscle to offload the patella-femoral joint (Tibial tuberosity osteotomy).
Prevention of developing chondromalacia patellae actually means reducing patient’s symptoms by avoiding provocative activities or positions of the knee
The risk of developing chondromalacia patellae can be prevented by following recommendations:
- Avoid repeated stress on the patella-femoral joint – squatting, kneeling, repeated use of stairs, prolonged standing, prolonged sitting, sitting on the floor or in a cross-legged position are avoided.
- Kneepads are advised if patients have to spend long time on their knees.
- Physiotherapy helps create muscle balance by strengthening patient’s quadriceps, hamstrings, abductors, and adductors. This single method proves very effective in the long run.
- Special knee tapings may be used by physiotherapists to improve patellar tracking and reduce pain
- Wear shoe inserts (insoles) that correct flat feet by increasing foot arch. This will decrease the amount of pressure placed on patient’s knees and may help realign the patella.
- Finally, excess body weight may stress patient’s knees. Maintaining a healthy body weight can help take pressure off the knees and other joints. Patients can take steps to lose their weight by reducing their sugar and fat intake, eating plenty of vegetables, fruits, and whole grains, and exercising for at least 30 minutes a day, five times a week.
All patients with chondromalacia patellae are thoroughly counselled right at the beginning about their recovery period. This can be anything between 6 to 12 weeks after starting treatment.
Physiotherapy is the main treatment. The patients are encouraged to be regular with their knee exercises and helped along to bear the initial increased knee pain. This improves patient’s co-operation and compliance with knee exercises.
With appropriate treatment, the patients should have rapid recovery and return to full functional level. The cartilage lesion may not heal itself, but the symptoms vanish. Patients are advised to follow certain precautions to avoid recurrence of their knee pain in the future.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

