Articular Cartilage Injuries
And Management
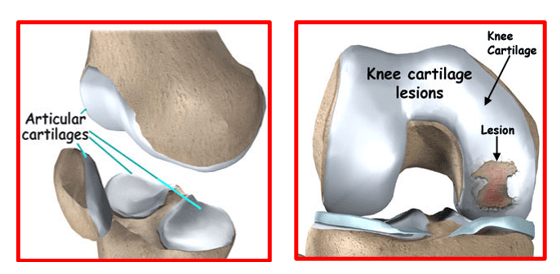
Articular cartilage is a highly specialised tough connective tissue that lines the ends of the bones where they articulate to form a joint. This lining (coating) consists of cells called chondrocytes in a matrix (scaffolding) of collagen fibres and proteins. It is firmly attached to the underlying bone. It allows the bones in a joint to move against one another with minimal friction.
The articular cartilage does not have any blood or nerve supply. It is white in colour due to lack of its own blood supply. It gets nourished by diffusion of nutrients through its tissue. Articular cartilage tissue is maintained and repaired by the cells contained within it. It is self-lubricating because of its high fluid content which gives it the lowest coefficient of friction of any natural or man-made material.
Injuries to the articular cartilage cannot heal themselves due to lack of blood supply. Lack of nerve supply means that patients may not feel any pain due to articular cartilage lesions until they become deep enough to load the underlying bone which has nerve supply.
Injuries or lesions of the articular cartilage can arise due to the following:
- Trauma (blunt impacts, traumatic patellar dislocation, polytraumatic injuries),
- Axial malalignment of the knee – causes overloading of affected area
- Fractures of the articular surfaces of the femur, tibia or patella
- Partial Total meniscectomy - increases stress in the affected compartment
- Instability (injuries to ACL, PCL, etc.) – can cause wear and tear at a younger age
- Osteochondritis dissecans – separation of articular cartilage with attached bone
- Osteoarthritis – age related wear and tear
- Rheumatoid arthritis – autoimmune disorder affecting multiple joints
- Genetic factors – arthritis runs into family affected several generations
- Obesity- overload of joints cause early wear
- Cartilage tumours
- Microtrauma- repeated micro-trauma and joint overloading causes arthritis
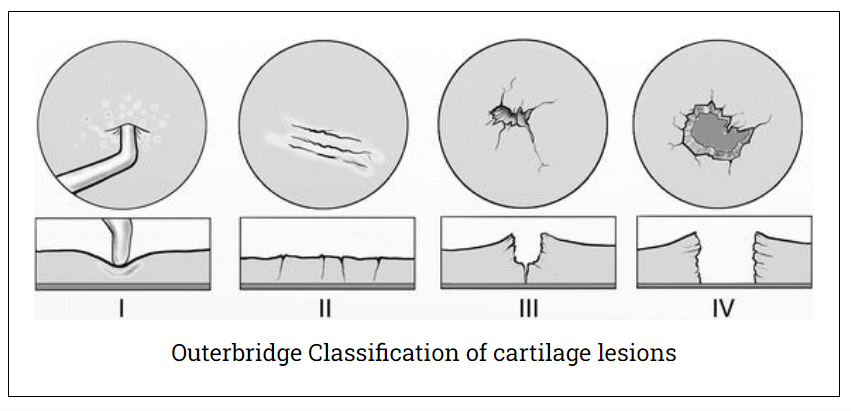
The grading system devised by Outerbridge is based on arthroscopy findings. It is simple and clinically useful in daily practice. It helps in understanding the severity of the articular cartilage lesion and also planning the most suitable treatment for these lesions.
Outerbridge’s Classification of Chondral Lesions:
- Grade 0 Normal articular cartilage
- Grade I Softening and blistering, or swelling of the cartilage
- Grade II Partial thickness defect with fissures and clefts,
not reaching subchondral bone, < 1.5 cm in diameter,
- Grade III Full thickness fissures, reaching subchondral bone,
> 1.5 cm in diameter
- Grade IV Exposed subchondral bone
Articular cartilage injuries most commonly occur in the knee joint, but the elbow, wrist, ankle, shoulder, and hip joints can also be affected.
In an acute scenario, the patients may present with pain, swelling, difficulty in walking and reduced knee joint mobility. They may also present with locking of the knee joint or may complain of their knee giving way. They may be limping whilst walking. These patients have a swollen and tender knee. There may be bruising around the knee joint. The knee movements are painfully limited. Patients may also show signs of any co-existing injuries like meniscal or ligament tears.
In the chronic stage, the patients may have pain, intermittent swelling, stiffness, sense of giving way or clicking sound. They may have episodes of their knee getting locked. Generally, the patient’s pain is aggravated while doing activities eg. stair climbing, squatting, kneeling, playing sports etc.
Articular cartilage injuries are diagnosed on the basis of detailed medical history, thorough clinical examination and appropriate investigations like knee X-rays and MRI scans.
X-rays do not show articular cartilage due to absence of calcium within its layers. But they will show the limb alignment (varus or valgus), presence of any loose bodies, fractures, reduction of joint space, calcification of meniscal cartilage, osteophyte (bony spurs) formation, tilting or mal-tracking of patella, defects in bones at joint level and presence of any cystic changes within the subchondral bones.
Magnetic Resonance Imaging (MRI)
Modern MRI scans give a detailed view of the articular cartilage itself and can bring out even smaller lesions. Several MRI scoring techniques have been focusing on size and location of the lesions and subchondral, cartilaginous, bony and meniscal abnormalities.
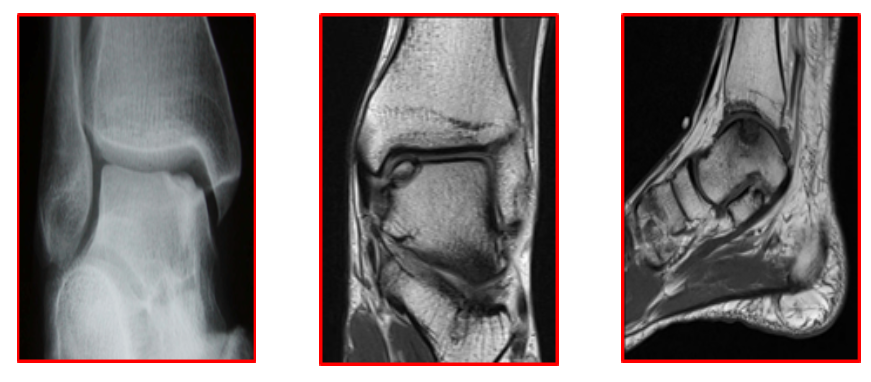
MRI imaging focuses on the following pathologies:
Cartilage defects (Location? Size? Depth?)
Injuries to the subchondral plate
Bony lesions (Osteochondritis Dissecans, fractures)
Secondary damages (ligament tears etc)
MRI is also very useful for planning the definitive treatment of patients with articular cartilage injuries.
Treatments for articular cartilage injuries are aimed at covering the defect area, either by cartilage regeneration or substitution, and allowing integration of this new cartilage with the native hyaline cartilage leading to improved joint function. These procedures should delay or prevent early wear and onset of osteoarthritis.
Surgical options include:
Arthroscopic Debridement –
Involves smoothing of the damaged cartilage and removing its loose edges to prevent it from rubbing and irritating other parts of the body. This arthroscopic procedure, known as chondroplasty, is done using small arthroscopic instruments, such as a mechanical shaver.
Loose bodies can also be removed by arthroscopically, and this will help reduce mechanical symptoms and may abolish locking or giving way of the joint. Areas of hypertrophic fibrillated cartilage can also be smoothed down using radiofrequency ablation probe.
Post traumatic large size loose bodies from weight bearing areas and having sufficient subchondral bone attached to it are ideally fixed with suitable implants.
This fixation can be done arthroscopically or by mini-open techniques. This allows bony union along with healing of the articular cartilage at its margins. Same principles can also be used for similar types of loose bodies arising due to osteochondritis dissecans.
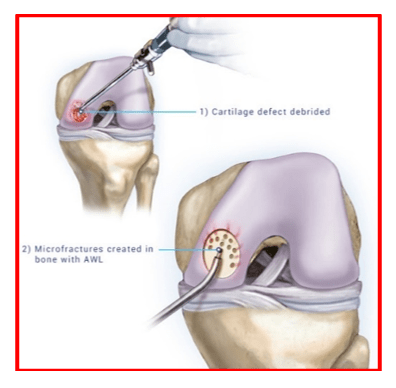
Marrow stimulation (Micro-fractures)
The goal of microfracture is to stimulate the growth of new articular cartilage by creating a new blood supply.
The best candidates are young patients with single lesions and healthy subchondral bone.
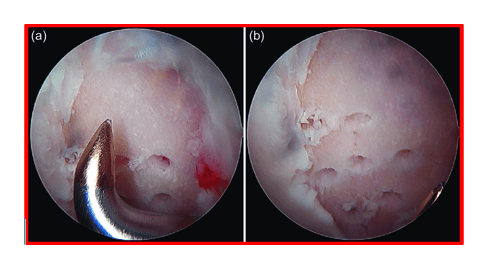
The surgeon makes tiny holes (micro-fractures) into the subchondral bone, under the damaged cartilage, with a sharp tool called awl. This procedure exposes the blood vessels that lie inside the bone. These micro-fracture holes cause localised bleeding and blood clot formation inside the cartilage defect area. Pluripotential stem cells from the marrow get recruited and the clot triggers the production of a new cartilage (called fibrocartilage) which grows and quickly fills up the defect area. Unfortunately, this new fibrocartilage is just like a specialised scar tissue and not a good replacement for the original hyaline cartilage. It is not as resilient to wear and lacks the characteristic low friction properties of hyaline cartilage. This means it wears away more quickly, and the patient may need further surgery later on in life.
In the later stages of articular cartilage wear, the bone eventually becomes exposed leading to increased friction, accelerated wear and the development of osteoarthritis.
Osteochondral Transfer
This procedure involves replacement of the cartilage defect with a substitute.
Osteochondral Autologous Transfer System (OATS):
Using a specialised drill, cylindrical plugs of cartilage with its attached underlying subchondral bone, are harvested arthroscopically from areas with relatively less weight bearing such as the intercondylar notch or the most lateral part of the femoral condyle. These plugs are then placed and matched to the surface area of the defect. Then these are impacted into place, in predrilled cylinders, leaving a smooth cartilage surface in the joint.
Osteochondral autograft is used for smaller cartilage defects, arising after trauma, in young patients (<50 years age).
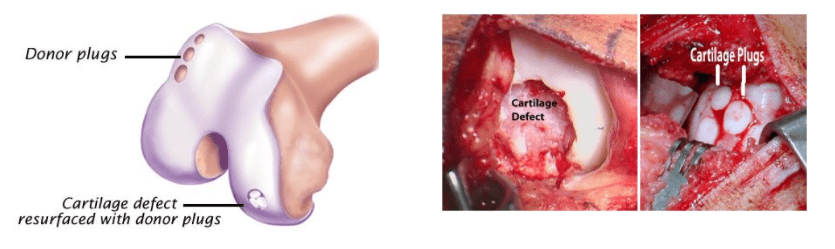
If multiple pieces are moved in this way to form a mosaic of new cartilage pieces in the damaged area, it is referred to as a Mosaicplasty.
It is not suitable when there is widespread cartilage damage, as seen in osteoarthritis.
Extensive Mosaicplasties have been largely taken over by newer methods of treatment such as Autologous Chondrocyte Implantation (ACI).
Autologous Chondrocyte Implantation (ACI):
This is a two-step procedure for biological cartilage regeneration.
New cartilage cells are first grown and then implanted in the cartilage defect. This technique allows filling up of large cartilage defect areas with hyaline cartilage.
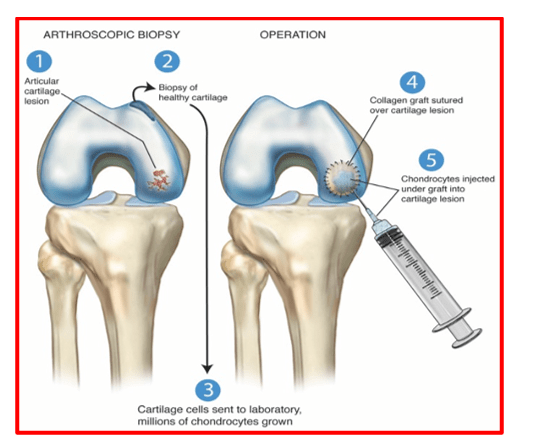
In the first stage, a small piece of cartilage is arthroscopically removed from a non-weight bearing region and sent to a laboratory. Here the chondrocytes are released by enzymatic digestion and expanded in culture medium to produce more cartilage cells (chondrocytes). The cells multiply and sufficient new cells are grown so that they can be used to cover the area of cartilage defect.
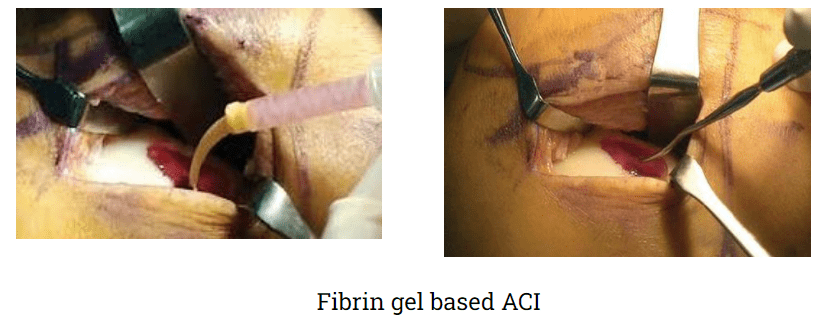
The second stage is done about 4 to 6 weeks later. The newly cultivated cartilage cells are implanted into the knee cartilage defect area, either by arthroscopic or mini-open techniques. During implantation, the cells are injected into the defect area after mixing with a fibrin-based gel. These implanted cells grow into healthy tissue. The new articular cartilage that grows is a hyaline cartilage and has same mechanical properties as the natural one.
ACI is most useful for younger patients who have single defects larger than 2 cm in diameter. ACI has the advantage of using the patient's own cells, so there is no danger of a patient rejecting the tissue. It does have the disadvantage of being a two-stage procedure that may requires an open incision for the second step. It also takes several weeks to complete.
Dr. Anand Jadhav uses a technique of Fibrin gel based ACI wherein the cultivated chondrocytes are mixed with a fibrin gel and used in the liquid state, to precisely fill the articular cartilage defect area. This mixture quickly solidifies. The chondrocytes trapped within the fibrin gel help in the healing of the cartilage lesion in a uniform manner.
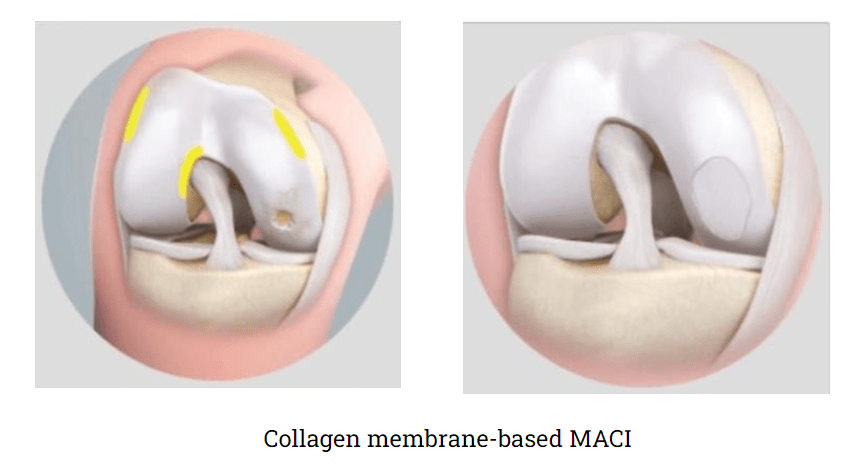
Matrix Guided Autologous Chondrocyte Implantation (MACI)
This technique has been developed to avoid problems associated with traditional ACI wherein chondrocytes were injected under a periosteal flap.This old technique lead to graft hypertrophy and uneven growth of the healthy cartilage.
In MACI, the cultured chondrocytes are first grown and then implanted in a scaffold (natural and synthetic biomaterials). This scaffold is then glued to the cartilage defect. This allows precise regrowth of the cartilage to fill up and cover the defect area.
Transplantation of Fresh Osteochondral Allografts:
Useful for large defects or defects located at odd locations and unsuitable for cartilage regeneration techniques or an autograft transfer.
An allograft is a tissue graft taken from a cadaver donor. Like an autograft, it is a block of cartilage and its underlying bone. In the laboratory the allograft is sterilized, prepared and tested for any possible disease transmission.
An allograft is typically larger than an autograft. It can be shaped to fit the exact contour of the defect and then press fit into place. Allografts are typically done through an open incision
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

