ACL Injuries & Management
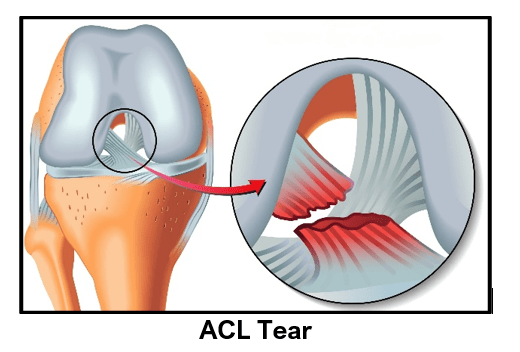
The anterior cruciate ligament (ACL) is one of the main restraining ligaments of the knee. The ACL is situated in the centre of the knee and runs from the back of the femur to the front of the tibia.
The ACL acts to prevent excessive forward movement of the tibia. It keeps the knee stable during rotational movements like twisting, turning or side-stepping activities.
Another important function of the ACL is to provide important neurological feedback about orientation of the one’s limbs in space. This perception is important for normal joint function in daily activities, occupational tasks and sports.
ACL is frequently injured in contact sports like football and pivoting sports like skiing. Non-contact twisting movement like side stepping, pivoting, landing from a jump can cause an ACL tear. ACL can also be injured in motorbike or car accidents due to sudden twisting of knee.
In acute stages:
- A popping sensation can be felt or heard during injury to ACL
- Swelling of the knee
- Pain in the knee
- Difficulty in weight bearing or walking
- Difficulty in bending the knee
In chronic stages:
- Sense of giving way & instability with twisting movements.
- Pain
- Swelling
Meniscal Injuries:either the outer (lateral) meniscus or inner (medial) meniscus or both can be injured.
Cartilage Injuries: The cartilage lining the femur, tibia or patella could be damaged. These cartilage lesions could be from minor flaps to major defects.
Ligament injuries: Medial collateral (MCL), lateral collateral (LCL) or Posterior cruciate ligament (PCL) injuries may also occur.
Fractures: could involve the tibia or femur.
ACL injury is diagnosed based on patient’s history of injury, symptoms and clinical examination. Special tests for ACL confirm excessive forward movement and also pivoting of tibia.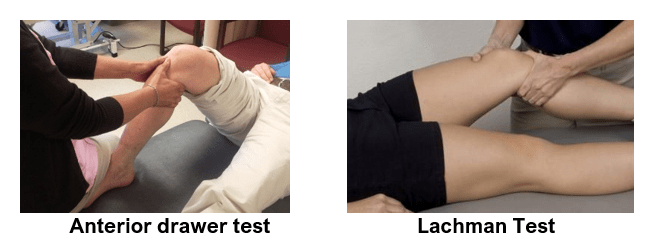
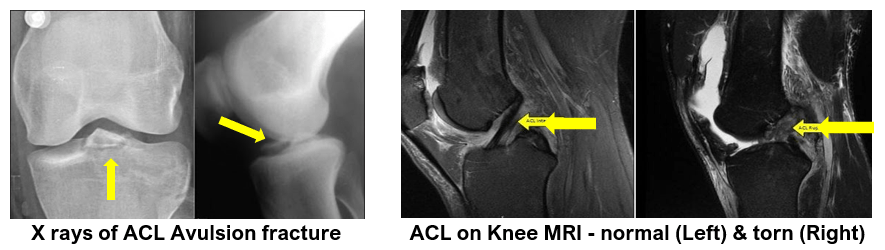
In acute cases, clinical examination is not possible due to pain and swelling. In such cases MRI is done to confirm the diagnosis.
A torn ACL is not seen on x-rays. But an x-ray may show any fractures around the knee joint, especially an avulsion of tibial spine where the ACL is attached to the shinbone.
The different types of ACL injuries are:
Grade I – Sprain (mild stretching) of the ACL fibres with some micro-tearing
of the ligament. There is no instability of the knee..
Grade II – ACL fibres are severely stretched with incomplete (partial) tears
of the ligament.
Knee is moderately unstable during stressful activities
Grade III – ACL fibres are completely torn. The ligament is unable to provide
stability to the knee joint
ACL avulsion fracture - this is a special type of ACL injury wherein the bony attachment of the ACL at the tibia is pulled off from the upper tibia. The ACL fires are not torn. This is also known as the tibial spine fracture. This fragment may be un-displaced or displaced.
Not all patients with ACL injury need surgery. You may choose not to have surgery if you:
- Have a minor tear in your ACL (a tear that can heal with rest and rehabilitation).
- Are not very active in sports and your work does not require a stable knee.
- Are willing to stop doing activities that require a stable knee or stop doing them at the same level of intensity. You may choose to substitute other activities that don't require a stable knee, such as cycling or swimming.
- Can complete a rehabilitation program that stabilizes your knee and strengthens your leg muscles to reduce the chances that you will injure your knee again and are willing to live with a small amount of knee instability.
- Do not feel motivated to complete the long and rigorous rehabilitation program necessary after surgery.
Conservative treatment of an ACL injury involves:
- Rest- from sports or heavy work
- Ice pack- to reduce swelling and pain
- Anti-inflammatory medications– reduce pain and inflammation. Allow patients to tolerate physiotherapy
- Strength– all muscles around the knee must be strengthened especially the hamstrings. These muscles can then take over some of the ACL’s role in knee stability.
- Balance and proprioception- as the ACL has an important role in providing information to the muscles and brain about the position of the knee joint, specific re-training of other nerves is performed to help compensate.
- Functional Knee Braces are may also be prescribed to help patients with damaged ACL’s. Their benefits are not fully understood although they may help with proprioception. They are expensive and may not provide much in the way of support to knee stability.
ACL reconstruction is recommended when you:
- Have completely torn your ACL or have a partial tear with an unstable knee
- Have gone through a rehabilitation program and your knee is still unstable.
- Are very active in sports or have a job that requires knee strength and stability (such as construction work), and you want your knee to be as strong and stable as it was before your injury.
- Are willing to complete a long and rigorous rehabilitation program.
- Have chronic ACL deficiency that is affecting your quality of life.
- Have a displaced ACL avulsion fracture
- Have injured other parts of your knee, such as the cartilage or meniscus, or other knee ligaments or tendons, that need surgery.
A knee with torn ACL has abnormal mobility of the tibia during normal activities and sports. This causes secondary damage to the joint cartilage and the meniscal tissues. Damage to the joint cartilage leads to knee arthritis at a younger age. The patients are not able to do active sports or lead a very active lifestyle due to instability and fear of knee buckling. ACL injury can be devastating and career threatening in an active athlete.
The goal of ACL surgery is to:
- restore normal or almost normal stability in the knee
- return you to the level of function you had before the knee injury
- limit loss of function in your knee
- prevent injury & degeneration of other knee structures e.g. the articular cartilage and the menisci.
- allow patients to lead an active lifestyle (includes sports and recreational activities)
The surgeries performed for treating various types of ACL injuries depend upon the type of ACL injury, the status of the ACL remnants or stumps (remains of the damaged ACL) and the time since injury.
Surgeons may perform any of the below mentioned procedures based on arthroscopic confirmation of ACL tears and their types:
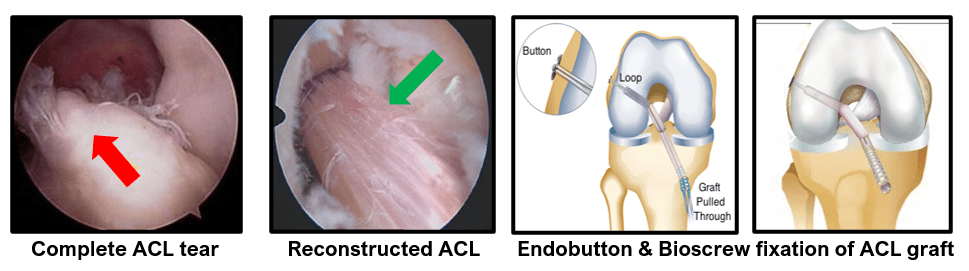
- Arthroscopic ACL Reconstruction – Gold Standard until now
- Arthroscopic Augmented ACL Reconstruction – rapidly gaining popularity
- Arthroscopic Primary Repair of ACL tear – for a select group of patients only
- Arthroscopic Primary ACL Repair with Augmentation
ACL reconstruction surgery is a surgical attempt to replace the stabilising function of the anterior cruciate ligament that has been injured. It is the commonest ligament reconstruction performed around the knee joint.
It involves removing the remains of the damaged ligament (ACL stumps) and replacing it with another form of soft tissue, called a graft.
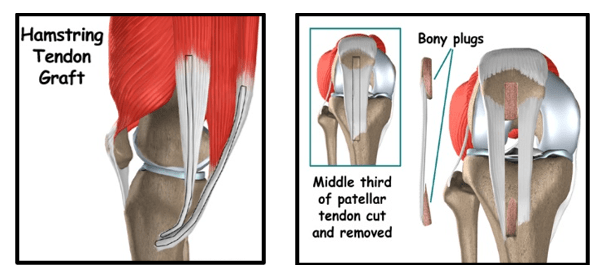
A number of grafts are available for use to replace the damaged ACL.
Grafts that are taken from patient’s own body are most popular. These are called the Autografts. These are usually harvested from the same side that is due for ACL reconstruction. In patients undergoing multi-ligament reconstructions or in some revision ACL cases, these autografts may be harvested from the patient’s opposite knee.
Grafts that are harvested from cadavers and then processed for use in patients are called Allografts. These allografts are needed occasionally in a select group of patients.
The two commonest graft techniques are to use the ‘hamstring tendons’ (soft tissue graft from the semitendinosus and gracilis muscle tendons) or the patella tendon graft, also called the Patellar tendon bone (PTB) or the Bone tendon bone (BTB) graft, that consists of a central strip of patellar tendon with bony plugs at either ends. The top plug comes from the lower patella and the bottom plug comes from the upper tibia.
Surgeons have also started using the Quadriceps tendon bone graft (QTB) from the front of the lower thigh with a bony plug of the upper patella and the entirely soft tissue graft of Peroneus longus tendon (PLT) from the outer side of the ankle.
ACL reconstruction surgery can be done by open technique or arthroscopically (through key holes) using telescope, camera and specialised instruments.
Dr Anand Jadhav has been trained, in all types of arthroscopic surgeries, by leading surgeons from the UK, Europe and the USA.
For the past 25 years, Dr Jadhav has been performing all types of ACL surgeries arthroscopically because arthroscopy offers:
- Excellent visualisation of structures in the knee joint
- Tiny scars and better cosmetic results
- Minimal tissue damage and bleeding
- Less pain
- Short hospitalisation
- Quicker rehabilitation
There is a 90 to 95% chance of a good result in patients who are having ACL surgery done for appropriate reasons and who comply with the rehabilitation plans of minimum 6 to 9 months. These patients have good muscle strength, knee stability and a painless range of motion. They can return to their pre-injury occupation or sports.
- This operation is done under general, spinal or epidural anaesthesia. A tourniquet is applied on the upper thigh in order to provide bloodless operating field.
- A telescope with attached camera and light source is introduced into the knee joint via two portals (tiny keyhole on either side of lower portion of the patella).
- Diagnostic arthroscopy is performed looking at all structures within the knee joint.
- Any meniscal or cartilage injuries are dealt with initially.
- Then the ACL tear is confirmed, and its type noted. The remnants/stumps of the torn ACL are thoroughly assessed. The decision to completely clear them or retain them depends upon the type of the ACL tear and the status of the torn or damaged tissue. If the stumps are very flimsy or poor quality, then they are cleared with a shaver from their attachments on the femur and tibia.
- Sites for inserting new ACL at tibial and femoral ends are clearly identified and marked. The remnants act as guides for placing the new bony tunnels.
- Hamstring tendon grafts (semi-tendinosis and gracilis) are harvested through a small incision on upper part of leg.
- The graft is then prepared to its thickest diameter and its length is noted. It is then covered with a vancomycin-soaked gauze and put under traction on the traction kit.
- Tibial and femoral bone tunnels of matching diameters and desired lengths are drilled with the help of special guides.
- The hamstring graft, with appropriate length marking, is now pulled into the knee joint through the tibial tunnel and then further upwards through the femoral tunnel.
- The femur side graft fixation is done either with an endo-button (a suspension device) or a metallic or absorbable screw. The graft is then tensioned with a special device to remove any slack during graft preparation.
- The tibial side fixation is done with either a metallic or absorbable screw.
- The new ACL is finally checked for - its position, tension, fixation strength and any signs of impingement (pinching or rubbing) against any bony part in the knee throughout its range of motion.
- The wounds are sutured or closed with sterile tapes. Sterile dressings are put on these wounds and a compression bandage is given.
- A hinged knee brace is applied at the end.
Augmented ACL Reconstruction is a technique where the torn or damaged portions of the native ligaments are left in place or minimally trimmed whilst reconstructing new ACL with any tendon graft.
Principles and Advantages of ACL Augmented Reconstruction:
- During ACL reconstruction surgery, the ACL stumps (remnants) act as definitive landmarks for creation of femoral and tibial tunnels precisely and thus enable anatomic ACL reconstruction
- The ACL remnants help in re-vascularisation and healing of the new graft. The graft healing and maturation processes are also accelerated
- The ACL remnants help in regrowth of nerves within the graft which gives better joint sense and provides knee stability (especially during early graft healing phase)
- This leads to faster rehabilitation and better functional recovery in such patients. They also have lower graft re-rupture rates.
- Additionally, specialised and strong suture materials can be used whilst preparing the new autografts. This step of augmenting the autograft with special tapes adds to the mechanical strength of the graft. It also provides early strength and protection to the new graft while it is healing. Patient can
be rehabilitated faster.
- Biologic augmentation intends to accelerate scar tissue healing (within the bony tunnels) and enable faster graft healing. It may alter the graft integration with the patient’s bones in a manner that resembles native ACL attachments. Platelet rich plasma (PRP) obtained from patient’s own blood is commonly used for this purpose. Its long-term effects are still awaited.
Yes, it is possible to repair a torn ACL in a select group of patients.
This procedure can be done by experienced surgeons in all age groups and for all types of indicated patients. It is showing very encouraging and better results than ACL reconstruction. This success of ACL repair is due to improved understanding of the native ACL anatomy and its biomechanics, improvement in modern fixation implants with strong suture materials and the development of stable fixation techniques
Primary Repair of an ACL tear is a technique where the ACL stump is reattached to the femur bone using specialised sutures and implants. This leads to healing of the torn ACL and preservation of the native ACL anatomy with all its functional advantages.
Primary ACL repair is indicated in the following circumstances:
- Proximal tear of the ACL with good tissue quality
- ACL injury with stump attached to PCL
- Isolated ACL injury
- Paediatric patients to avoid injury to their growth plates
- Multi-ligament knee injuries
Advantages offered by Primary ACL repair:
- No graft harvesting needed
- Native ligament biology and blood supply preserved
- Offers near normal knee kinematics
- Rehabilitation can be fast tracked and early return to sports becomes possible
- Slows down progression of knee towards arthritis compared to ACL reconstruction
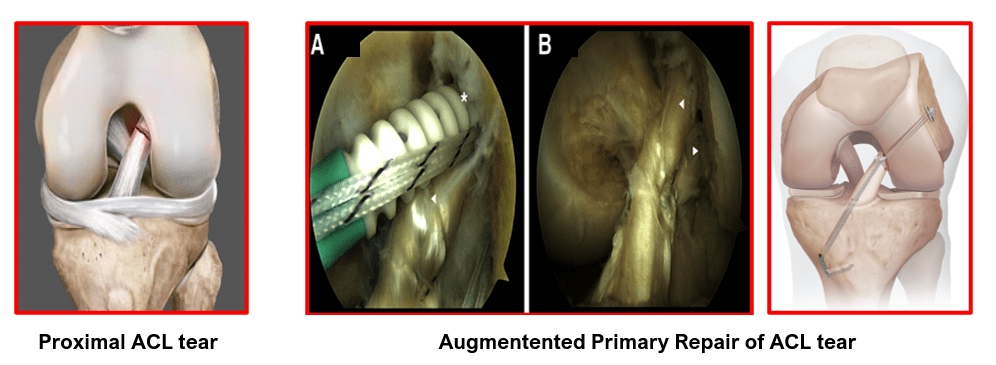
- Tissue tape augmentation of Primary ACL Repair provides better stability during the repair stages. It protects the ligament from necrosis and ligamentisation. The graft healing is faster.
- This construct is biomechanically superior to non-augmented repair
Your hospital stay will be 1-2 days
Patients can start walking or moving the knee on the same day of the operation or the next day. They usually need the help of elbow crutches or a walker initially to help in mobilization. You will be given instructions about the type of exercises to be done for the next 3 months. These exercises will be monitored weekly by our physiotherapist. My team will guide you through your recovery period.
I recommend that you continue physiotherapy for a minimum of 3 months to regain normal range of knee motion, good muscle strength and sense of stability (proprioception) in the knee joint. Patient are then encouraged to continue their rehabilitation further for 6 to 9 months in a stepwise manner to gain maximum benefits from the ACL reconstruction.
During the first 3 months, there is healing of the soft tissue graft within the bony tunnels of the tibia and femur. At this time, the graft is at its weakest point strength wise, as it is undergoing structural remodelling.
Over the next 6 to 9 months the graft gradually strengthens. It regains its original strength only after 9 to 12 months have passed since the ACL reconstruction surgery. This process, of graft remodelling and strengthening, is known as ligamentisation of the graft.
Regular physiotherapy is hence needed to take patients to the next level of workout intensity at regular fixed intervals. This advancement is as per the improvement in their strength and the time elapsed since their ACL surgery.
Patients who comply with full rehabilitation programme have a very high chance of a good result. Knee stability is restored, joint is fully mobile, and the patients can undertake most of the normal activities, including sports.
If a patient tries to get back to high intensity activities or sports, before the tendon healing and transformation process is completed (i.e. before 9 months), there is a very high chance of rupturing or tearing the new graft as it is still weak.
We take all efforts in counselling our ACL reconstruction patients about this process of healing of the new graft and its gradual strengthening over a long period.
You will need crutches for 2- 4 weeks depending on your progress.
You need to use the knee brace for 4-6 weeks depending on your progress
The sutures are removed 10-12 days after the surgery.
For office-type jobs you can return to work after 1- 2 weeks and for other heavy intensity jobs after 3 months, provided the progress is satisfactory.
You can drive a car after 4-6 weeks and ride a motorbike after 6-8 weeks. Your knee should be pain-free with good range of motion, strength and stability.
Generally, any sort of sporting activities, are restricted for 6 to 9 months.
Full intensity sports are allowed after 9 months of rehabilitation.
Like any other surgical procedure ACL Reconstruction has following risks:
The risks of any anesthesia are:
Allergic reactions to medicines
Breathing problems
The risks of any surgery are:
Bleeding
Infection
Additional risks of this surgery are:
Stiffness of the knee
Failure of the ligament to heal
Failure of graft fixation devices
Pain in the knee
Weakness of the knee
Blood clot in the leg
Injury to a nearby blood vessel, nerves or tendon
Numb area on outer side of knee
Difficulty with kneeling
Fracture of patella if patellar tendon graft is used.
Rupture of new ligament if knee is injured again.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

