Achilles Tendon
and Its Disorders
The Achilles tendon is a tough band of fibrous tissue that connects the calf muscles to the heel bone (calcaneus). The Achilles tendon is also called the calcaneal tendon.
The gastrocnemius and soleus muscles of the calf unite to form a band of tissue at the low end of the calf. This band travels down to insert into the back of the calcaneum (heel bone). Small sacs of fluid called bursae cushion the Achilles tendon at the heel.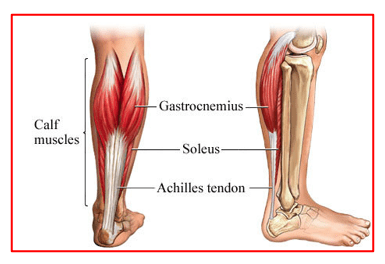
The Achilles tendon is the largest and strongest tendon in the body. When the calf muscles contracts, the Achilles tendon pulls on the heel and allows it to move downwards (plantar flexion). This movement allows us to stand on our tip toes. This lifting of the heel (push off) is needed when walking, running, or jumping.
The Achilles tendon, though very strong, is vulnerable to injury, due to its limited blood supply and the high tensions placed on it. Achilles tendon problems are very common and range from tendinitis and tendinosis (inflammation and degeneration of the tendon itself) to complete ruptures of the tendon.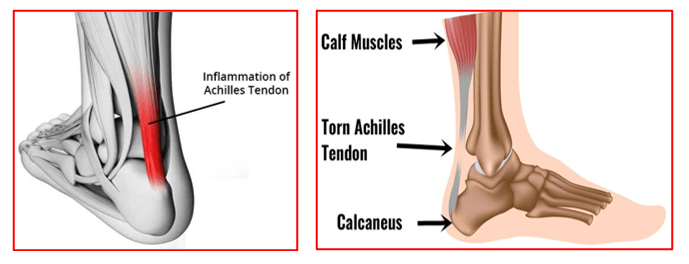
- Achilles tendinitis (tendonitis): Frequent activity (running or walking) can gradually inflame the end of the Achilles tendon, causing pain and stiffness at the back of the heel.
- Achilles peritendonitis: Similar to Achilles tendonitis, but inflammation and pain occur in the tissue surrounding the tendon, often two or more inches above the heel. In acute cases, the tendon appears like a sausage due to the severe swelling. Commonly seen in long distance runners. Pain comes with activities and settles with rest.
- Achilles tendinosis: Gradual thickening of the Achilles tendon without apparent inflammation, due to aging or overuse. There is tendon degeneration with loss of its normal structure and also tendon thickening.
Despite the thickening, the tendon is weakened and prone to further injury or rupture. Aging plus repetitive minor trauma, such as playing sports that involve running or jumping, without proper healing can also play a role. Areas of tendinosis may eventually progress to partial or complete ruptures if they experience high loads, especially during push-off and landing activities in sports like football or basketball.
- Achilles or heel (calcaneal) bursitis: This is a movement related swelling and inflammation of the retrocalcaneal bursa (lubricating sac), the fluid-filled cushioning sac between the heel bone and the Achilles tendon. Low-riding shoes or an injury can irritate the bursa and make it painful. This pain is localised the front of the Achilles tendon, in the area between the tendon and the heel bone. The bursa can become inflamed or thickened and stick to the tendon, as a result of overuse or repetitive loading. Pain and tenderness can come from squeezing the tendon itself or the space just in front of the tendon.
- Insertional achilles tendonitis involves inflammation at the point where the Achilles tendon inserts into the heel bone. People with this condition often have tenderness directly over the insertion of the Achilles tendon, which is commonly associated with calcium formation or a bone spur forming just above the insertion point. This condition can occur along with retrocalcaneal bursitis (see below) and a bony enlargement of the heel bone, known as Haglund’s deformity. This deformity occurs in women who wear high-heeled shoes or men and women hockey players because of the skate rubbing on the back of the heel.
- Partial or complete tears / ruptures of the achilles tendon: these tears can arise due to acute trauma or chronic overuse
Achilles tendon problems are diagnosed on the basis of patient’s medical history, clinical examination and investigations.
Patients have pain around their ankle region at the back for long duration. This can occur after activities like running or walking. They may have difficulty in climbing stairs or standing tip toes. They may develop a limp whilst walking. Patients are unable to carry on high intensity activities or sports. They have a swollen, tender and deformed achilles tendon. There is weakness of plantar flexion or downward movement of the ankle on stressing.
Investigations help the surgeon in confirming the exact diagnosis and severity of the achilles tendon problems.
X-ray film: A plain X-ray film may identify problems with the bones or ankle joint, but it cannot diagnose Achilles tendon problems.
MRI: is the best test to diagnose an Achilles tendon rupture or other problems but it may not always detect tendinopathy.
Calf and ankle ultrasound: Ultrasound can often diagnose an Achilles tendon rupture. It is a dynamic test and can allow to see how the tendon in the tendon closes after bending the foot downwards.
Achilles tendinitis can be managed predominantly by conservative measures. Surgery may be needed occasionally.
Conservative measures include:
- Rest: Avoid putting weighton your leg as best you can. You may need crutches to offload the ankle region.
- Ice packs: are to be used for 4 to 5 times daily for about 20 mins each time.
- Leg Compression: Using an elastic bandage around the lower leg and ankle helps to keep the down swelling.
- Leg elevation: Patients are encouraged to keep their affected leg up on a pillow whenever they are sitting or lying down. This helps to reduce swelling and pain.
- Anti-inflammatory painkillers: These help in reducing pain and swelling.These are taken as required for limited period of time only to avoid medication related complications like stomach ulcers or kidney problems.
- Heel raise/cushions: these keep the ankle in a downward position and ease the tension on the inflamed tendon. It prevents further stretching on the inflamed tendon. Thus, pain is reduced, and mobility improved. Needs to be used on both feet for proper balancing whilst walking.
- Physiotherapy: Stretching and strengthening exercises are started. These help to regain strength & mobility at the ankle joint and also improves its function. Additional modalities like, ultrasound therapy, matrix therapy or laser therapy may be used to reduce, tendon swelling and pain and improve local blood supply to assist in tendon healing.
- Platelet rich plasma injection (PRP): This is derived from patient’s own blood. It helps in directly delivering platelet derived growth factors at the site of tendon lesion and promote healing of the tendon. This relieves pain & swelling of the achilles tendon. These injections have now replaced the corticosteroid injections which, though cheap and helpful, were associated with delayed achilles tendon ruptures.
Surgery:
Surgery is advised if a patient fails to respond to the conservative measures or he ruptures his achilles tendon. These surgeries may be for debridement of the inflamed tendon and or repair of partial /complete tendon ruptures.
Arthroscopic surgery: for excision of Haglund’s deformity is commonly performed. The enlarged bone and the overlying inflamed bursa are removed arthroscopically. The deep portion of the achilles tendon, gets inspected at the same time.
Open surgery: is used for large size Haglund’s deformity to excise the bone, to remove the diseased portion from within the achilles tendon and to repair the achilles tendon to the calcaneum.
Achilles tendon rupture is a common injury. Rupture usually occurs in the section of the tendon situated within 5 to 6 cm from the point where the tendon attaches to the heel bone. This section might be prone to rupture because blood flow is poor, which also can impair its ability to heal.
Ruptures often are caused by a sudden increase in the stress on the Achilles tendon. e.g.
- Participating in sports that involve jumping, running and cutting activities
- Falling from a height
- Stepping into a hole
Some risk factors are also associated with achilles tendon rupture:
- Age:The peak age for Achilles tendon rupture is 30 to 40 years.
- Sex:Achilles tendon rupture is up to five times more likely to occur in men than in women.
- Recreational sports:Achilles tendon injuries occur more often during sports that involve running, jumping, and sudden starts and stops — such as football, basketball and tennis.
- Steroid injections: injections near ankle joint can predispose patients for rupture of their achilles tendon
- Certain antibiotic:Fluoroquinolone antibiotics, such as ciprofloxacin or levofloxacin increase the risk of Achilles tendon rupture.
Obesity: Excess weight puts more strain on the tendon.
The most common initial symptom of Achilles tendon rupture is a sudden snap at the lower calf, intense pain, and inability to point the foot downward.
Patients feel a pop and often feel like someone has kicked them in the back of the leg when they rupture their achilles tendon. Along with intense pain, they may have swelling and bruising around the heel region. They are limping and have difficulty in walking. Patients are not able to stand on their tip toes.
There is local tenderness and a palpable gap at the rupture site. Squeezing the calf fails to move the foot downwards.
Achilles tendon tear is diagnosed on the basis of patient’s medical history, clinical examination and investigations.
Investigations help the surgeon in confirming the exact location of the tear and the status of the tendon.
X-ray film: A plain X-ray film may identify problems with the bones or ankle joint, but it cannot diagnose Achilles tendon problems.
MRI: is the best test to diagnose an Achilles tendon rupture or other problems but it may not always detect tendinopathy.
Calf and ankle ultrasound: Ultrasound can often diagnose an Achilles tendon rupture. It is a dynamic test and can allow to see how the tear in the tendon closes after bending the foot downwards.
Achilles tendon tears can be treated with conservative or surgical methods.
Treatment choice depends on patient’s age, activity levels and the severity of their tendon tear.
Conservative treatment is advised for older people, less active people, smokers, diabetics and those with partial achilles tendon tears.
Conservative treatments:
- Rest
- Painkiller medications are taken as and when required
- Ice packs are done if using a leg splint or walker boot.
- Leg elevation over 2 pillows is encouraged to keep leg above the level of the heart. This helps in reducing swelling and pain.
- Plaster cast – A below knee plaster cast is applied with ankle and toes pointing in downwards position. This ensures that the torn tendon edges are well approximated and assist in tendon healing. Patients can walk toe touch weight bearing with help of a walker or elbow crutches. Early weight bearing helps in tendon healing as well as its maturation. Plaster gets changed every two weeks to gradually bring the foot into a neutral position and allow normal full weight bearing after 4 weeks.
- Ankle walker boot – used with heel wedges to keep the ankle and toes pointing downwards. Used as an alternative to the plaster cast. Height of the heel wedges within the walker boot is gradually reduced every 2 weeks. Patients are allowed to weight bear as tolerated just like with a plaster cast.
Conservative treatment avoids the risk of wound infection but takes longer time for recovery and has a slightly higher tendon re-rupture rate.
The total protection needed, either with a plaster cast or a walker boot is 8 weeks.
Surgery:
Surgical repair of the achilles tendon is advised for younger, active and sports persons with complete achilles tendon tears. Surgical repair helps in getting back the correct length of the tendon. The tendon re-rupture rates are also lower compared with conservative treatment. Surgery helps athletes to return to their pre-injury status and high intensity activities. But surgery does have issues of wound healing, infection & scar tenderness.
The procedure generally involves making an incision over the lower leg at the rupture site and stitching the torn tendon ends together with strong nonabsorbable sutures. Depending on the condition of the torn tendon tissue and time since injury, the repair might be reinforced with other tendons.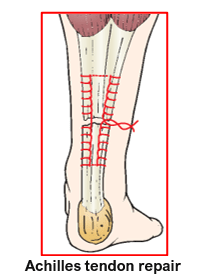
Patients with achilles tendon injury need to follow a structured physiotherapy rehabilitation programme that helps to keep the ankle joint supple, avoid ankle stiffness and help in healing and maturation of the healing tendon. A pair of elbow crutches or a walker is used for support when mobilising.
After surgery, patients are given a plaster cast in equinus (ankle and toes pointing downwards) or a walker boot with heel wedges, to protect the tendon repair. This position keeps the repaired tendon ends together and eases tension on the tendon. The downward angle of immobilisation gets changed gradually at 2 weeks & 4 weeks mark to bring the foot upwards.
0 to 2 weeks: Toe touch weight bearing as tolerated is started from next day of surgery.
2 to 4 weeks: Partial weight bearing is started after change of angle of the plaster cast or walker boot. The foot is brought up short of normal. 4 to 6 weeks: Full weight bearing is started.
At 6 weeks: Plaster cast is removed. The ankle is further immobilised for another 2 to 4 weeks in an ankle walker boot in neutral position.
Full weight bearing is allowed along with ankle range of motion to regain normal mobility and ankle strength. Physiotherapy is to be continued on OPD basis for 3 to 4 months.
6 to 12 months: Return to sports or high intensity activities can be possible after structured rehabilitation for several months. This avoids avoid re-rupture of the tendon that normally occurs with premature and early return to sports.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday, Wednesday & Friday 7 PM to 9 PM
Sunday 11 AM to 1 PM
Appointments
London Joints Clinic ( PCMC )
Address
C/O Dr Nitin’s Physio Clinic,
Opp. Brahma Hotel,
Near Akurdi Post Office,
Vivek Nagar,
Akurdi,
Pune 411035
Saturdays only 4.30 PM to 7.30 PM
Appointments
Hospitals OPDs : Locations & Directions
Manipal Hospital

Address
Manipal Hospital, Opp D Mart, Baner-Mhalunge Road, Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

