Posterior Tibial
Tendon Dysfunctions
The posterior tibial (PT) tendon is one of the major stabilising structures in the foot. It runs behind the bump on the inside of the ankle (the medial malleolus) and inserts into one of the bones of the instep (navicular). The main functions of the tendon are to support the arch of the foot and keep the foot turned inwards when walking.
Posterior tibial tendon dysfunction, also known as acquired flatfoot, is one of the most common deformities of the foot and ankle. This occurs when the posterior tibial tendon is acutely torn, or it becomes degenerative due to wear and tear.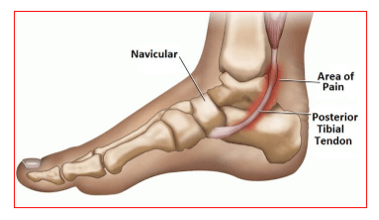
The tendon gradually weakens and stretches, resulting in the flattening of the arch of the foot. This condition is progressive and can lead to a rigid flatfoot over time with arthritic changes.
Posterior tibial tendon dysfunction is more common in females and in those in their sixth decade.
The risk factors associated with posterior tibial tendon dysfunction are:
- Obesity
- Hypertension
- Diabetes
- Increased age
- Use of corticosteroids
- Sero-negative inflammatory disorders
The symptoms of posterior tibial tendon dysfunction are:
- Pain initially along the course of the posterior tibial tendon (behind the medial malleolus and at its insertion onto the navicular bone)
- Painful limp
- Difficulty in walking or weight bearing
- Swelling along the posterior tibial tendon region
- Loss of the arch of the foot
- In later stages, there is pain on the outer border of the foot and fixed flatfoot deformity of the hindfoot
Posterior tibial tendinitis is diagnosed based on patient’s medical history, symptoms, thorough clinical examination and investigations.
Patients walk with a limp. They have flat foot which make be flexible or rigid. There will be tenderness along the tendon course and the surrounding joints. Patients are unable to do a single limb heel raise.
The foot may be deformed in advanced stages.
X-rays of the ankle and foot are taken. These will show flattening of the arch, any bony deformities and arthritis changes. Help assess the severity of the deformity.
MRI of the ankle and foot show the status of the tendon and the severity of arthritic changes at the hindfoot and midfoot joints.
Ultrasound helps in dynamic assessment of the tendon pathology and its quality.
The posterior tibial tendon dysfunction can be managed conservatively or surgically based on the stage of the problem.
Conservative treatment is used for early or mild stages and consists of:
- Painkiller medications
- Rest and avoiding high intensity activities
- Walking aids – pair of elbow crutches or a walker
- Insoles with medial arch support
- Appropriate fitting shoes for walking and outdoor activities
- Ankle walker boot with arch support
- PRP injections – helps in healing of the inflamed tendon
Surgical management: used for torn tendon or advanced stages of posterior tibial tendon dysfunction or arthritis of the affected joints
Teno-synovectomy & Tendon repair/reconstruction – is indicated for patients who fail to respond to above conservative measures in very early stages of the tendon dysfunction.
The tendon sheath is opened up and the diseased portion cleaned up. The weakened tendon may be repaired and additionally strengthened by using the flexor digitorum longus (FDL) tendon which lies alongside the posterior tibial tendon at the ankle.
To improve the biomechanics of the tendon transfer, the heel bone is moved towards the inside of the foot (calcaneal osteotomy), held with one screw. A plug is also inserted into the subtalar joint to support the arch. The plug and screw are generally removed in a second operation when the tendon is strong enough, about 6 months after the first operation. This is a small day case operation and recovery is swift.
For advanced stages –
3 of the foot joints can become arthritic. These joints (subtalar, talonavicular, and calcaneocuboid) are fused using bone graft taken from either the heel or the hip bone. This is known as a triple fusion.
The recovery from tendon reconstruction or fusion surgery is very lengthy. Patients will spend 6 weeks in a cast and remain non-weight bearing for 6 weeks. They are taught to mobilise with elbow crutches or a walker. They need to undergo an intensive rehabilitation programme as directed by their physiotherapist. Patients are advised an ankle walker boot for an additional 6 weeks after their first cast gets removed.
X-rays are done at 6 weeks and 12 weeks mark to assess bony fusion status. Patients are left free without any ankle support after 3 months when their foot and ankle x-rays confirm complete fusion.
Book An Appointment
Private Clinics : Locations & Directions
London Joints Clinic (Pune)
Address
Office S 5, 2nd Floor, North Block, Sacred World Mall,
Opp Sacred Heart Township, Near Jagtap Chowk,
Wanawadi, Pune 411040
Monday to Saturday
6 PM to 9 PM
Appointments
Hospitals OPDs : Locations & Directions
Jupiter Hospital (Baner)

Address
Lane 3, Baner- Balewadi Road,
Prathamesh Park,
Baner, Pune 411 045
Monday to Saturday 11 AM to 4 PM
Appointments
Contact us
Dr Anand Jadhav has a centralised appointment system for all locations across various hospitals and clinics in Pune & PCMC areas
Appointment Bookings & Requests can be made by any method :

